
Gynaecology is the medical practice dealing with the female health and its reproductive systems (vagina, uterus and ovaries) and the breasts. It means "the science of women".
Here the consultation for all women health related problems is offered with evidence based treatment and women is also provided with the information which aims to help women make informed decisions about the treatment choices . The most common problems dealt are;

• Excessive menstrual bleeding affects one in five women. The amount of blood lost in each period in terms of the amount, length, and frequency of bleeding. A heavy period for one woman may be normal for another.
• Menstrual bleeding is defined as heavy (and call it menorrhagia) when periods last longer than seven days or more than 80ml of blood is lost during a period. However, the way that a woman perceives the heaviness of her period is as important as any clinical measurements.
When menstrual bleeding is heavy, clotting can also occur. Losing large clots can be extremely upsetting and even painful if they are large because they can cause cramping as they pass through the cervix.
• If your periods have changed, it's very important to see doctor.The doctor will investigate possible causes and offer the appropriate treatment.
• But in about half the women with heavy bleeding, no cause can be found.
• Some causes of heavy menstrual bleeding
o Fibroids - these benign (not cancerous) growths in the muscular wall of the uterus are a common cause of heavy bleeding.
o Polyps - these benign growths of the lining of the uterus may cause heavy bleeding but more commonly lead to spotting between or after periods.
o Pelvic inflammatory disease - an infection in the reproductive tract which can cause infertility and chronic pain if untreated.
o Endometriosis - a painful condition in which the lining of the uterus grows outside the uterus.
o Endometrial hyperplasia - thickening of the lining of the uterus, leading to heavier bleeding.
o Endometrial cancer - cancer of the lining of the uterus, causing heavy periods, bleeding between periods and blood-stained vaginal discharge. Rare, but more common in women after the menopause.
o Hormone Imbalances - can stop ovulation (egg release) leading to build-up of endometrium and heavier periods.
o Hypothyroidism - an underactive thyroid gland can cause heavier periods.
o Blood clotting disorders.
o Use of anticoagulant drugs. Unexplained - for half of all cases no cause can be found.
o Contraceptive coil (IUD) – multiload or copper T coil can cause heavier, longer periods.
• Millions of women in India suffer from the problem of heavy bleeding during their periods. This not only causes extreme inconvenience, discomfort, loss of work days and exclusion from religious activities but also severe weakness and anaemia.
• Many of these women in their 30’s and 40’s are suffering from dysfunctional uterine bleeding (DUB) where the womb (Uterus) is normal, yet they have heavy menses.
• Endometrial sampling may be suggested to rule out cancer or precancerous condition of uterine lining .
• Medical science developments have made medicines which are having excellent results in management of heavy menses..
• A simple, non surgical method of treating heavy menses is to insert a hormonal intrauterine device (LNG _ IUD). This is a small shaped T ’device, which looks like a Copper T or loop but has hormone inside it. This can be placed inside the uterus in five minutes, usually without any anaesthesia and once inside the womb, it reduces or stops bleeding during menses for a period of 5 years in most of the patients. This also gives contraceptive benefit to women . This is a temporary method and the device can be removed at any time.
• This device is simple and safe and gives good results in well selected patients, though results may take time to reflect in terms of cyclic flow and pain.

• Painful periods (dysmennorhoea) is common problem in teenagers and many girls miss school and college because of it. This is usually due to excessive local production of prostaglandin’s and can be reduced by light exercise, hot showers and antiprostaglandin and analgesic tablets taken at the onset of menses.
• Menstrual hygiene is very important and must be taught to all young girls. Frequent baths during the periods, changing pads frequently, disposing off the pads hygienically is absolutely necessary. Even today, there are lots of myths about menstruation like not eating pickle, not entering the kitchen, taking total rest during this time etc., all of which are illogical.
• Many girls experience bloating, breast pain, depression and irritability prior to menses and the symptoms disappear after the periods. This is perfectly normal and restriction of salt, refined flour, caffeine and chocolates along with light exercise during this time helps relieve symptoms.
• Also addition of calcium, B-complex, primrose oil and such supplements may help reduce symptoms.
• In some women, hormonal pills have to be given if there is severe pain.
• Other causes mainly, fibroid ,infection or abnormal shape of uterine cavity can be ruled out with a routine checkup and abdominal sonography.

• The early initial periods can be very irregular and may not become regular upto 12 – 18 months of starting. This is due to immaturity of the hormone axis and is normal.. Gradually the menses will normalize and the girl will bleed for 3 – 5 days every 28-30 days, which is the normal cycle.
• Menstruation usually begins anytime between 9-14 years. If onset of menses is delayed beyond this, examination and tests of the girl are required to confirm that there is no problem.
• Amenorrhea is the absence of menstruation — one or more missed menstrual periods. Women who have missed at least three menstrual periods in a row have amenorrhea, as do girls who haven't begun menstruation by the age of 16.
Other disorders that can cause irregular menses are:
• Polycystic ovarian syndrome – the ovaries develop clusters of blister-like cysts. Symptoms include irregular periods and excessive hair growth. Women with polycystic ovarian syndrome are especially prone to amenorrhoea when they gain weight.
• High levels of male sex hormones, which can affect the reproductive system. This can be caused by ovarian or adrenal tumours, or certain conditions present at birth.
• High levels of the breastfeeding hormone prolactin. Levels rise due to overactivity of, or a tumour on, the pituitary gland.
• Ovarian failure or early menopause – low levels of oestrogen cause ovulation to fail, which stops the menstrual cycle.
• pregnancy tests, which can be either a urine or a blood test
• physical examination to determine overall health and the presence of other sexual characteristics
• medical history, including gynaecological history and contraceptive methods used
• hormone tests to check the functioning of the thyroid, ovaries, ,hypothalamus and pituitary glands
• Ultrasound of the reproductive system.
• Treatment is to manage the underlying disorder.
• If the condition is due to extreme weight, treatment will involve encouraging you to maintain a healthier body weight.
• Hormone replacement therapy (HRT), such as the combined oral contraceptive pill, will usually cause periods to return, but will not treat any underlying cause.

• Vaginal discharge serves an important housekeeping function in the female reproductive system. Fluid made by glands inside the vagina and cervix carries away dead cells and bacteria. This keeps the vagina clean and helps prevent infection.
• Most of the time, vaginal discharge is perfectly normal. The amount can vary, as can odor and hue (its color can range from clear to a milky white-ish), depending on the time in your menstrual cycle. For example, there will be more discharge if you are ovulating, breastfeeding, or are sexually aroused. The smell may be different if you are pregnant or you haven't been diligent about your personal hygiene.
• None of those changes is cause for alarm. However, if the color, smell, or consistency seems significantly unusual, especially if it accompanied by vaginal itching or burning, you could be noticing an infection or other condition.
What causes abnormal discharge?
• Any change in the vagina's balance of normal bacteria can affect the smell, color, or discharge texture. These are a few of the things that can upset that balance:
• Antibiotic or steroid use
• Bacterial vaginosis, a bacterial infection more common in pregnantwomen or women who have multiple sexual partners
• Birth control pills
• Cervical cancer
• Chlamydia or gonorrhea (STDs), sexually transmitted infections
• Diabetes
• Douches, scented soaps or lotions, bubble bath
• Pelvic infection after surgery
• Pelvic inflammatory disease (PID)
• Trichomoniasis, a parasitic infection typically contracted and caused by having unprotected sex
• Vaginal atrophy, the thinning and drying out of the vaginal walls during menopause
• Vaginitis, irritation in or around the vagina
• Yeast infections.
• How you are treated will depend on what’s causing the problem. For example, yeast infections are usually treated with antifungal medications inserted into the vagina in cream or gel form. Bacterial vaginosis is treated with antibiotic pills or creams. Trichomoniasis is usually treated with the drug metronidazole (Flagyl) or tinidazole .Here are some tips for preventing vaginal infections that can lead to abnormal discharge:
• Keep the vulva clean by washing regularly with a gentle, mild soap and warm water.
• Never use scented soaps and feminine products or douche. Also avoid feminine sprays and bubble baths.
• After going to the bathroom, always wipe from front to back to prevent bacteria from getting into the vagina and causing an infection.
• Wear 100% cotton underpants,
• Avoid overly tight clothing.
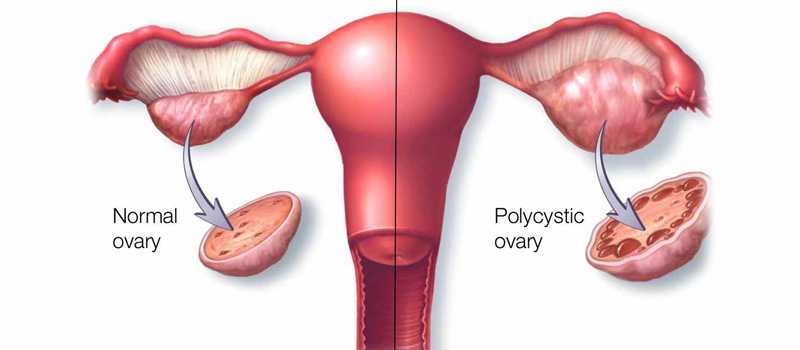
Polycystic ovary syndrome (PCOS) is a health problem that affects one in 10 women of childbearing age. Women with PCOS have a hormonal imbalance and metabolism problems that may affect their overall health and appearance. PCOS is also a common and treatable cause of infertility.
Polycystic ovary syndrome (PCOS), is a common health problem caused by an imbalance of reproductive hormones which creates problems in the ovaries. The ovaries make the egg that is released each month as part of a healthy menstrual cycle. With PCOS, the egg may not develop as it should or it may not be released during ovulation as it should be.
PCOS can cause missed or irregular menstrual periods. Irregular periods can lead to:
• Infertility (inability to get pregnant). In fact, PCOS is one of the most common causes of female infertility.
• Development of cysts (small fluid-filled sacs) in the ovaries.
Some of the symptoms of PCOS include:
• Irregular menstrual cycle. Women with PCOS may miss periods or have fewer periods (fewer than eight in a year). Or, their periods may come every 21 days or more often. Some women with PCOS stop having menstrual periods.
• Too much hair on the face, chin, or parts of the body where men usually have hair. This is called "hirsutism." Hirsutism affects up to 70% of women with PCOS.3
• Acne on the face, chest, and upper back
• Thinning hair or hair loss on the scalp; male-pattern baldness
• Weight gain or difficulty losing weight
• Darkening of skin, particularly along neck creases, in the groin, and underneath breasts
• Skin tags, which are small excess flaps of skin in the armpits or neck area
Yes. Having PCOS does not mean you can't get pregnant. PCOS is one of the most common, but treatable, causes of infertility in women. In women with PCOS, the hormonal imbalance interferes with the growth and release of eggs from the ovaries (ovulation). If you don't ovulate, you can't get pregnant.
Our treatment plan can help you ovulate and to raise your chance of getting pregnant
Yes, studies have found links between PCOS and other health problems, including:
• Diabetes. More than half of women with PCOS will have diabetes or pre-diabetes (glucose intolerance) before the age of 40.
• High blood pressure.
• Unhealthy cholesterol.
• Sleep apnea.
• Depression and anxiety.
• Endometrial cancer. Problems with ovulation, obesity, insulin resistance, and diabetes (all common in women with PCOS) increase the risk of developing cancer of the endometrium (lining of the uterus or womb).
There is no single test to diagnose PCOS.
• Physical Exam. blood pressure, body mass index (BMI), and waist size, skin for extra hair on your face, chest or back, acne, or skin discoloration.
• Pelvic exam.
• Pelvic ultrasound (sonogram). This test uses soundwaves to examine your ovaries for cysts and check the endometrium (lining of the uterus or womb).
• Blood tests. Blood tests check your androgen hormone levels, sometimes called "male hormones.” and thyroid disease, may also test your cholesterol levels and test you for diabetes.
There is no cure for PCOS, but you can manage the symptoms of PCOS.
• Doctor will work on a treatment plan based on your symptoms, your plans for children, and your risk for long-term health problems such as diabetes and heart disease.
You can take steps at home to help your PCOS symptoms, including:
• Losing weight. Healthy eating habits and regular physical activity can help relieve PCOS-related symptoms.
• Losing weight may help to lower your blood glucose levels, improve the way your body uses insulin, and help your hormones reach normal levels.
• Even a 10% loss in body weight (for example, a 150-pound woman losing 15 pounds) can help make your menstrual cycle more regular and improve your chances of getting pregnant.
PCOS can cause problems during pregnancy for you and for your baby. Women with PCOS have higher rates of
• Miscarriage
• Gestational diabetes
• Preeclampsia
• Cesarean section (C-section)
Your baby also has a higher risk of being heavy (macrosomia) and of spending more time in a neonatal intensive care unit (NICU).
You have several options to help your chances of getting pregnant if you have PCOS:
• Losing weight. If you are overweight or obese, losing weight through healthy eating, including eating the right amount of calories for you, and regular physical activity can help make your menstrual cycle more regular and improve your fertility.
• Medicine. After ruling out other causes of infertility in you and your partner, we might prescribe medicine to help you ovulate.
• Surgery. Surgery is also an option, usually only if the other options do not work. The outer shell (called the cortex) of ovaries is thickened in women with PCOS and thought to play a role in preventing spontaneous ovulation. Ovarian drilling is a surgery in which the doctor makes a few holes in the surface of your ovary using lasers or a fine needle heated with electricity. Surgery usually restores ovulation, but only for six to eight months

The overactive bladder means that your bladder contracts (squeezes) when you do not want it to.
This is the probable reason for your frequent and urgent need to pass urine. It can also cause leakage of urine because you cannot get to the toilet in time.
We can help you to improve this, providing we have your co-operation and you have determination. The purpose of bladder training is to help you regain control of your over-active bladder by suppressing its contractions.
You must gradually increase the capacity of your bladder and the time interval between voiding (passing water).
Start by voiding every hour on the hour whether you need to or not, from when you get up in the morning until you go to bed at night, but try very hard not to void at any other time, that is, in between your set times. Practice this for 3–4 days. When you feel you have mastered this, gradually extend the time between voiding.
This type of leakage tends to occur when the woman coughs, sneezes, lifts, runs or walks fast.
The leakage is due to a weakness of the pelvic floor that supports the bladder and the urethra (the tube which comes from the bladder to the outside).
You will be given advice on restricting the amount of fluid you drink, stopping smoking, reducing your weight and doing pelvic floor exercises.
In approximately 1 in every 3 women these non-operative treatments are sufficient to cure or make your symptoms very much better.
However, many women still require an operation to improve the quality of their life.
Operations for stress incontinence depend on supporting the urethra. The main operation to cure this type of leakage is Sling operation. Of the patients who have the operation, stress incontinence is cured in 85%, improved in a further 10% and not helped in approximately 5%.
Why have a repair?
As women get older, especially if they have had children, the muscles and supporting tissues of the pelvic floor (around the vagina) can become lax.
This can cause ‘prolapse’ of the walls of the vagina and/or the uterus (womb).
Problems women get with prolapse are:-
• A lump coming down
• Difficulty passing urine
• Difficultly opening bowels
Vaginal operations are usually very good at relieving the symptoms of a lump coming down and have variable effects on urinary and bowel symptoms.
What is a repair?
This operation involves an incision within the vagina and repair of the underlying connective tissue.
• This takes up some of the laxity in the vaginal walls.
• If your womb is prolapsed you may be offered a ‘vaginal hysterectomy’ at the same time.
• Pelvic Floor Exercises for Women
What are pelvic floor muscles?
• They are layers of muscles , helping to hold the bowel, bladder and uterus in place and closing the outlets of the bladder and bowel.
• When you pass urine or have a bowel motion, the pelvic floor muscles relax. After emptying, they tighten again to restore control.
Why do pelvic floor exercises?
• Weakness of the pelvic floor muscles can be a common problem affecting 1 in 3 women by middle age, resulting in incontinence and prolapse.
• This may be due to being overweight, post pregnancy/childbirth, pelvic surgery or simply getting older.
• Incontinence can affect your bladder and/or bowel. So if you: „ leak on coughing, sneezing, laughing or physical exertion „ leak before reaching the toilet „ are of child-bearing years „ are menopausal pelvic floor exercises are for you.
• Identifying the pelvic floor muscles .
Stage 1:
Tighten your back passage – imagine that you are stopping yourself passing wind, focus on the tightening around the opening of the bowel. Do not squeeze your buttocks or leg muscles.
Stage 2:
your vagina and front passage – imagine that you are trying to stop the flow of urine. Focus on this tightening; try to feel the muscles lifting upwards and forwards towards the pubic bone.
Stage 3:
• Do both of the above tightening exercises together and hold this. How many seconds can you hold? Aim for 5 seconds – when you let go, can you feel the muscles relax? If not, you have held too long – try again with a shorter hold. Some women may be able to hold for only 1-2 seconds and others as many as 8-10 seconds. It is important to discover your hold.. Repeat this 10 times – approximately 1 contraction per second.
• Do not expect immediate improvement – so do not give up.
• You need to continue this routine for at least 6 months.
• As the muscle gets stronger you will be able to increase your hold and number of repetitions at each session.
• Do not practice stopping midstream.
• Exercise for life Continue pelvic floor exercise several times per day for the rest of your life in order to keep these muscles fit and healthy.
• If symptoms return increase your daily input again.
• Additional tips Being constipated or overweight can strain the pelvic floor muscles so eat a balanced diet including fruit and vegetables and between 6 and 8 cups of fluid a day.
• Avoid tea, coffee or coca-cola if you suffer from urgency or frequency.
• Tightening the pelvic floor muscles when you lift heavy objects or when you are going to cough or sneeze will help your control.
• If your problem is ‘urgency’, tighten your pelvic floor when you get the desire to empty your bladder, wait until the desire passes before moving.
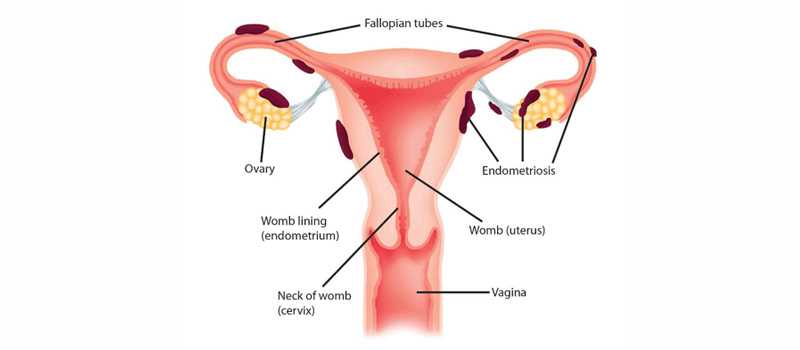
Endometriosis is a condition where the cells that form the lining of the uterus grow into the surrounding areas. Aside from pain, especially during menstruation, during and after intercourse, it can also cause infertility.
About a third of all cases of female infertility are caused by endometriosis where the excess cells occur in the fallopian tubes and block the egg’s passage, or they occur in the ovaries and prevent the release of the egg, or they form in the uterus, ovaries and fallopian tubes and prevent the transfer of the egg to the tube.
Endometriosis is usually treated in one if three ways: watchful waiting, hormone therapy and surgery, depending on your symptoms, age, severity and if fertility is a factor.
The purpose of surgery is to remove as many endometrial implants and cysts as possible, which would relieve pain and improve fertility, and is recommended for women who are still in the child bearing age. It can be done via laparoscopy or laparotomy.
Laparoscopy is the gold standard and preferred method for endometriosis surgery. This is a day care procedure, and you do not need to stay in hospital overnight. Recovery usually takes a 1 -2 weeks.
In a Laparotomy, which is only considered in cases of severe endometriosis, the specialist accesses your reproductive organs through a large incision across your abdomen.

• Every women should visit her gynaecologist from time to time, even if healthy. The purpose of these visits is to:
• Screen for medical issues
• Assess your risk for future medical problems
• Encourage a healthy lifestyle
• Update vaccinations
• Help you get to know your provider in case of an illness
• There are specific times when you should consult your gynaecologist. Below are screening guidelines for women ages 18 to 39.
• PHYSICAL EXAM
Screening for cervical cancer should begin at age 21.
• BREAST SELF-EXAM AND MAMMOGRAM
• Women may do a monthly breast self-exam
• Screening mammogram is not recommended for most women under age 40.
• Women ages 40 to 44 should have the choice to start annual breast cancer screening with mammograms (x-rays of the breast) if they wish to do so. Women age 45 to 54 should get mammograms every year. Women 55 and older should switch to mammograms every 2 years, or can continue yearly screening.
• If you have a mother or sister who had breast cancer at a young age, consider yearly mammograms. They should begin earlier than the age at which their youngest family member was diagnosed.
• If you have other risk factors for breast cancer, we may recommend a mammogram, breast ultrasound, or MRI scan.
• DIABETES SCREENING
If you have a body mass index (BMI) greater than 25 and have other risk factors for diabetes, you should be screened. Asian Americans should be screened if their BMI is greater than 23.
•IMMUNIZATIONS
• Cervical cancer vaccine
• Know about the human papilloma virus (HPV) vaccine if you are between ages 10 to 45 and you have:
• Not received the HPV vaccine in the past (you will need all three shots)
• Not completed the full vaccine series (you should catch up on this shot)
• You should get a flu shot every year.
• Contact if you notice a change in your breasts, whether or not you do breast self-exams.
• If you are between ages 20 to 40, we may do a clinical breast exam.
• PELVIC EXAM AND PAP SMEAR
• Beginning at age 21, women should have a pelvic exam and Pap smear every 3 years to check for cervical cancer.
• If you are over age 30 and your Pap smear and HPV test are normal, you only need a Pap smear every 5 years.
• If you have had your uterus and cervix removed (total hysterectomy) and you have not been diagnosed with cervical cancer you may not need to have Pap smears.
• OTHER SCREENING
• Routine bone density screening of women under 40 is not recommended.
• Do I Need to Do Anything to Prepare for a Pelvic Exam?
• Because a Pap test is typically performed during a routine pelvic exam, you should schedule the exam when you are not having your period .In addition, for 48 hours prior to the exam, you should not:
• Douche
• Use a tampon
• Have sex
• Use birth control foam, cream, or jelly
• Use medicine or cream in your vagina
• What Can I Expect During a Pelvic Exam?
• You can expect to feel a little discomfort, but you should not feel pain during a pelvic exam. The exam itself takes about 10 minutes.
• Perform a smear or liqid based cytology (LBC).We will use a plastic spatula and small brush to take a sample of cells from the cervix (A sample of fluid also may be taken from the vagina to test for infection.)
Patients Younger Than 21 Years
The first visit to the obstetrician–gynecologist for screening and the provision of preventive services and guidance take place between the ages of 13 years and 15 years. This visit generally does not include pelvic examination. The focus of this visit should be on patient education. During this visit, the obstetrician–gynecologist can establish the clinician–patient relationship and engage in age-appropriate discussion of anatomical development, body image, self-confidence, weight management, immunizations (including the human papillomavirus vaccine), contraception, and prevention of STIs .

Why it's done?
• Cancer cervix is the most common cancer in women and is highly common in India, taking lives of many women every year.
• Fortunately, Nature has given us provision to visually inspect this internal organ and the potential to check the possibility of cancer ,years before it actually begins by means of simple test Pap smear or LBC.
• A Pap smear is used to screen for changes in a sample of cells that may precede cervical cancer. The Pap smear is usually done in conjunction with a pelvic exam.
• In women older than age 30, the Pap test may be combined with a test for human papillomavirus (HPV) — a common sexually transmitted infection that can cause cervical cancer in some women.
What is pap and LBC test?
• A Pap smear, also called a Pap test, is a procedure to test for cervical cancer in women. A Pap smear can also detect changes in your cervical cells that suggest cancer may develop in the future.
• A Pap smear involves collecting cells from your cervix — the lower, narrow end of your uterus that's at the top of your vagina.
• Detecting cervical cancer early with a Pap smear gives you a greater chance at a cure. Detecting these abnormal cells early with a Pap smear is your first step in halting the possible development of cervical cancer.
• Liquid based cytology: Instead of cells being smeared onto a glass slide, they are washed into a vial of liquid and filtered, and a random sample is presented in a thin layer on a glass slide. These slides can then either be screened by skilled staff or subjected to partially automated imaging.
Who should have a Pap smear?
• As every women can potentially develop cancer in cervix, Pap test is recommended for all sexually active women.
• In general, doctors recommend beginning Pap testing at age 21 or when you begin sexually active life.
• Your doctor can decide when it's time for you to begin Pap testing and how often you should have the test.
How often should Pap smear be repeated?
• Doctors generally recommend repeating Pap testing every 3 years for women ages 21-65.
• Women age 30 and older can consider Pap testing every 5 years if the procedure is combined with testing for HPV.
• If you have certain risk factors, your doctor may recommend more-frequent Pap smears, regardless of your age. These risk factors include:
• A diagnosis of cervical cancer or a Pap smear that showed precancerous cells
• HIV infection
• Weakened immune system due to organ transplant, chemotherapy or chronic corticosteroid use
• You and your doctor can discuss the benefits and risks of Pap smears and decide what's best for you based on your risk factors.
Who can consider stopping Pap smears?
• In certain situations a woman and her doctor may decide to end Pap testing, such as:
• After a total hysterectomy. After a total hysterectomy — surgical removal of the uterus including the cervix — ask your doctor if you need to continue having Pap smears.
• If your hysterectomy was performed for a noncancerous condition, such as uterine fibroids, you may be able to discontinue routine Pap smears.
• But if your hysterectomy was for a precancerous or cancerous condition of the cervix, your doctor may recommend continuing routine Pap testing.
• Older age. Doctors generally agree that women can consider stopping routine Pap testing at age 65 if their previous tests for cervical cancer have been negative.
• Discuss your options with your doctor and together you can decide what's best for you based on your risk factors. If you're sexually active with multiple partners, your doctor may recommend continuing Pap testing.
Risks
• A Pap smear is a safe way to screen for cervical cancer. However, a Pap smear isn't foolproof. It's possible to receive false-negative results — meaning that the test indicates no abnormality, even though you do have abnormal cells.
• A false-negative result doesn't mean that a mistake was made. Factors that can cause a false-negative result include:
• An inadequate collection of cells
• A small number of abnormal cells
• Blood or inflammatory cells obscuring the abnormal cells
• Although it's possible for abnormal cells to go undetected, time is on your side. Cervical cancer takes several years to develop. And if one test doesn't detect the abnormal cells, the next test most likely will.
How you prepare yourself for pap test?
• To ensure that your Pap smear is most effective, follow these tips prior to your test:
• Avoid intercourse, douching, or using any vaginal medicines or spermicidal foams, creams or jellies for two days before having a Pap smear, as these may wash away or obscure abnormal cells.
• Try not to schedule a Pap smear during your menstrual period. Although the test can be done, it's best to avoid this time of your cycle, if possible
• Cervical cells
During the Pap smear
• A Pap smear is performed in your doctor's office and takes only a few minutes.
• Your doctor will gently insert an instrument called a speculum into your vagina. The speculum holds the walls of your vagina apart so that your doctor can easily see your cervix. Inserting the speculum may cause a transient sensation of mild pressure in your pelvic area.
• Then your doctor will take samples of your cervical cells using a soft brush or a flat scraping device called a spatula. This usually doesn't hurt.
After the Pap smear
• After your Pap smear, you can go about your day without restrictions.
• Depending on the type of Pap testing you're undergoing, your doctor transfers the cell sample collected from your cervix into a container holding a special liquid to preserve the sample (liquid-based Pap test) or onto a glass slide (conventional Pap smear).
• The samples are transferred to a laboratory where they're examined under a microscope to look for characteristics in the cells that indicate cancer or a precancerous condition.
• Ask your doctor about when you can expect the results of your test.
• Results
• A Pap smear can alert regarding the presence of suspicious cells that need further testing.
Normal results
If only normal cervical cells were discovered during your Pap smear, you're said to have a negative result. You won't need any further treatment or testing until you're due for your next Pap smear and pelvic exam.
Abnormal Results
• If abnormal or unusual cells were discovered during your Pap smear, you're said to have a positive result. A positive result doesn't mean you have cervical cancer. What a positive result means depends on the type of cells discovered in your test.
• Here are some terms your doctor might use and what your next course of action might be:
Atypical squamous cells of undetermined significance (ASCUS). Squamous cells are thin and flat and grow on the surface of a healthy cervix. In the case of ASCUS, the Pap smear reveals slightly abnormal squamous cells, but the changes don't clearly suggest that precancerous cells are present.
• With the liquid-based test, we can get to reanalyze the sample, to check for the presence of viruses known to promote the development of cancer, such as some types of human papillomavirus (HPV).
• If no high-risk viruses are present, the abnormal cells found as a result of the test aren't of great concern. If worrisome viruses are present, you'll need further testing.
• If the changes are high grade, there's a greater chance that the lesion may develop into cancer much sooner. Additional diagnostic testing is necessary.
• Further testing is needed to determine the source of the abnormal cells and their significance.
• If your Pap smear is abnormal, we may perform a procedure called colposcopy using a special magnifying instrument (colposcope) to examine the tissues of the cervix, vagina and vulva.
• We may take a tissue sample (biopsy) from any areas that appear abnormal. The tissue sample is then sent to a laboratory for analysis and a definitive diagnosis

• Colposcopy is a very helpful procedure to closely examine your cervix, vagina and vulva for signs of disease.
During colposcopy, your doctor uses a special magnifying instrument called a colposcope.
• The most common reasons why colposcopy is performed include:
• The presence of abnormal cells as confirmed by a cervical screening sample, regardless if these cells are cancerous or not
• The patient is diagnosed with human papillomavirus or HPV, a leading cause of abnormal cell changes leading to cervical cancer
• Inconclusive cervical screening tests
• Certain symptoms raising suspicions of an unhealthy cervix, including vaginal bleeding and cervical inflammation
The colposcopist will be able to tell right away if there are abnormalities, so there is no need to wait for the results of the test.
However, if a biopsy is performed after the Colposcopy, 40% of patients who were required to undergo colposcopy obtained abnormal results.
However, an abnormal result does not necessarily mean that the patient has cervical cancer, but the presence of the abnormal cells point to an increased risk of cancer especially if the abnormality is not treated right away. A colposcopy, however, may be able to diagnose a cervical cancer; in such cases, the patient is quickly referred to a cancer specialist.
Normal results mean that the cervix is healthy and the patient has a low risk of developing cervical cancer. Regardless of the results, women are encouraged to undergo cervical screening test every three to five years as a preventative measure.
• Digital Colposcopy is done at suprabhat healthcare center and the procedure typically takes 10 to 20 minutes.
• You'll lie on your back on a table with your feet in supports, just as during a pelvic exam or Pap test.
• Your doctor positions the special magnifying instrument, called a colposcope, a few inches away from your vulva. A bright light is shined into your vagina, and your doctor looks the magnified and focused view, on the computer screen.
• Cervix and vagina are swabbed with cotton to clear away any mucus. We may apply a solution of vinegar or another type of solution to the area. This may cause a burning or tingling sensation. The solution helps highlight any areas of suspicious cells.
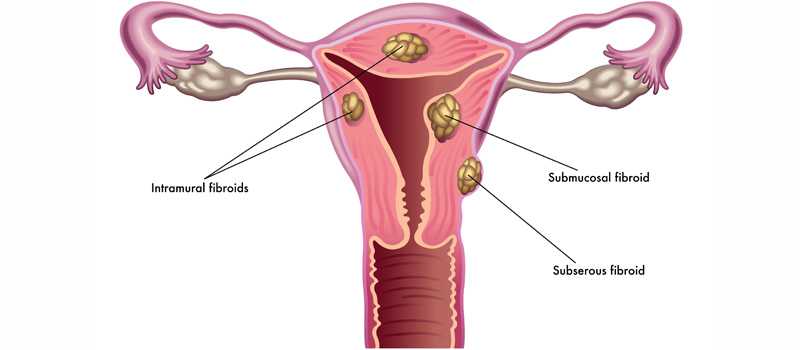
• Fibroids are abnormal growths that develop in or on a woman’s uterus. Sometimes these tumors become quite large and cause severe abdominal pain and heavy periods. In other cases, they cause no signs or symptoms at all. The growths are typically benign, or noncancerous. The cause of fibroids is unknown.
• Fibroids are also known by the following names:
• leiomyomas
• myomas
• uterine myomas
• fibromas
• According to the National Institutes of Health (NIH), about up to 80 percent of women have them by the age of 50. However, most women don’t have any symptoms and may never know they have fibroids.
What are the different types of fibroids?
The type of fibroid a woman develops depends on its location in or on the uterus.
• Intramural fibroids
Intramural fibroids are the most common type of fibroid. These types appear within the muscular wall of the uterus. Intramural fibroids may grow larger and can stretch your womb.
• Subserosal fibroids
Subserosal fibroids form on the outside of your uterus, which is called the serosa. They may grow large enough to make your womb appear bigger on one side.
• Pedunculated fibroids
Subserosal tumors can develop a stem, a slender base that supports the tumor. When they do, they’re known as pedunculated fibroids.
• Submucosal fibroids
These types of tumors develop in the middle muscle layer, or myometrium, of your uterus. Submucosal tumors aren’t as common as the other types.
What causes fibroids?
It’s unclear why fibroids develop, but several factors may influence their formation.
• Hormones
Estrogen and progesterone are the hormones produced by the ovaries. They cause the uterine lining to regenerate during each menstrual cycle and may stimulate the growth of fibroids.
• Family history
Fibroids may run in the family. If your mother, sister, or grandmother has a history of this condition, you may develop it as well.
• Pregnancy
Pregnancy increases the production of estrogen and progesterone in your body. Fibroids may develop and grow rapidly while you’re pregnant.
Who is at risk for fibroids?
• Women are at greater risk for developing fibroids if they have one or more of the following risk factors:
• pregnancy
• a family history of fibroids
• age of 30 or older
• a high body weight
What are the symptoms of fibroids?
• Your symptoms will depend on the number of tumors you have as well as their location and size. For instance, submucosal fibroids may cause heavy menstrual bleeding and trouble conceiving.
• If your tumor is very small or you’re going through menopause, you may not have any symptoms. Fibroids may shrink during and after menopause. This is because women undergoing menopause are experiencing a drop in their levels of estrogen and progesterone, hormones that stimulate fibroid growth.
Symptoms of fibroids may include:
• heavy bleeding between or during your periods that includes blood clots
• pain in the pelvis or lower back
• increased menstrual cramping
• increased urination
• pain during intercourse
• menstruation that lasts longer than usual
• pressure or fullness in your lower abdomen
• swelling or enlargement of the abdomen
How are fibroids diagnosed?
For a proper diagnosis, you’ll need to see a gynecologist to get a pelvic exam. This exam is used to check the condition, size, and shape of your uterus. You may also need other tests, which include:
•Ultrasound
An ultrasound uses high-frequency sound waves to produce images of your uterus on a screen. This will allow your doctor to see its internal structures and any fibroids present. A transvaginal ultrasound, in which the ultrasound wand is inserted into the vagina, may provide clearer pictures since it’s closer to the uterus during this procedure.
•Pelvic MRI
This in-depth imaging test produces pictures of your uterus, ovaries, and other pelvic organs.
How are fibroids treated?
• Your doctor will develop a treatment plan based on your age, the size of your fibroids, and your overall health. You may receive a combination of treatments.
• Managing your stress levels and losing weight if you’re overweight can also benefit women with fibroids.
• Medications to regulate your hormone levels may be prescribed to shrink fibroids. Gonadotropin-releasing hormone (GnRH) agonists, such as leuprolide (Lupron), will cause your estrogen and progesterone levels to drop. This will eventually stop menstruation and shrink fibroids.
• Other options that can help control bleeding and pain, but won’t shrink or eliminate fibroids, include:
• an intrauterine device (IUD) that releases the hormone progestin
• over-the-counter (OTC) anti-inflammatory pain relievers, such as ibuprofen (Advil)
• birth control pills
• Surgery to remove very large or multiple growths may be performed. This is known as a myomectomy. An abdominal myomectomy involves making a large incision in the abdomen to access the uterus and remove the fibroids. The surgery can also be performed laparoscopically, using a few small incisions into which surgical tools and a camera are inserted. Fibroids might grow back after surgery.
• If your condition worsens, or if no other treatments work, your physician may perform a hysterectomy. However, this means that you won’t be able to bear children in the future.
Minimally invasive procedures
Another surgical option is uterine artery embolization. In this procedure, small particles are injected into the uterus in order to cut off the fibroids’ blood supply.
What can be expected in the long term?
• Your prognosis will depend on the size and location of your fibroids. Fibroids may not need treatment if they’re small or don’t produce symptoms.
• If you’re pregnant and have fibroids, or become pregnant and have fibroids, your doctor will carefully monitor your condition. In most cases, fibroids don’t cause problems during pregnancy. Speak with your doctor if you expect to become pregnant and have fibroids
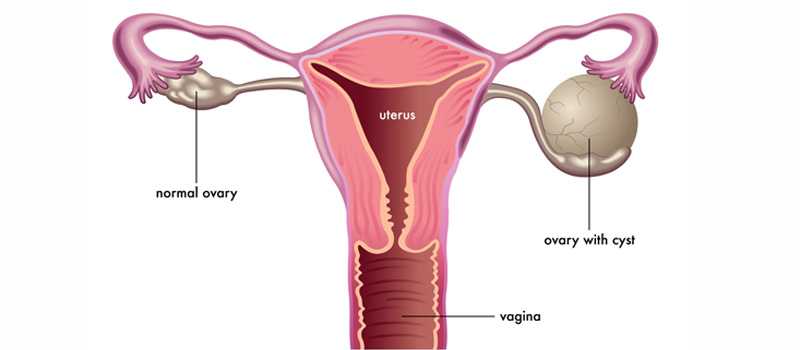
• The ovaries are part of the female reproductive system. They’re located in the lower abdomen on both sides of the uterus. Women have two ovaries that produce eggs as well as the hormones estrogen and progesterone.
• An ovarian cyst is a larger fluid-filled sac (more than 3 cm in diameter) that develops on or in an ovary. A cyst can vary in size from a few centimetres to the size of a large melon. Many women will develop at least one cyst during their lifetime. In most cases, cysts are painless and cause no symptoms
• Ovarian cysts may be thin-walled and only contain fluid (known as a simple cyst) or they may be more complex, containing thick fluid, blood or solid areas.
• An ovarian cyst is a fluid-filled sac that develops on a woman's ovary. They're very common and don't usually cause any symptoms.
• Most ovarian cysts occur naturally and disappear in a few months without needing any treatment.
• The ovaries
• The ovaries are two small, bean-shaped organs that are part of the female reproductive system. A woman has two ovaries – one each side of the womb (uterus).
• The ovaries have two main functions:
• to release an egg approximately every 28 days as part of the menstrual cycle
• to release the female sex hormones, oestrogen and progesterone, which play an important role in female reproduction
• Ovarian cysts may affect both ovaries at the same time, or they may only affect one.
• An ovarian cyst usually only causes symptoms if it splits (ruptures), is very large, or blocks the blood supply to the ovaries.
• In these cases, you may have:
• pelvic pain – this can range from a dull, heavy sensation to a sudden, severe and sharp pain
• pain during sex
• difficulty emptying your bowels
• a frequent need to urinate
• heavy periods, irregular periods or lighter periods than normal
• bloating and a swollen tummy
• feeling very full after only eating a little
• difficulty getting pregnant – although fertility is unaffected in most women with ovarian cysts (see ovarian cysts and fertility)
• See your GP if you have persistent symptoms of an ovarian cyst.
• The two main types of ovarian cyst are:
• functional ovarian cysts – cysts that develop as part of the menstrual cycle and are usually harmless and short-lived; these are the most common type
• pathological ovarian cysts – cysts that form as a result of abnormal cell growth; these are much less common
• Ovarian cysts can sometimes also be caused by an underlying condition, such as endometriosis.
• The vast majority of ovarian cysts are non-cancerous (benign), although a small number are cancerous (malignant). Cancerous cysts are more common in women who have been through the menopause.
• ultrasound scan, carried out by using a probe placed inside your vagina.
• If a cyst is identified during the ultrasound scan, you may need to have this monitored with a repeat ultrasound scan in a few weeks, or your GP may refer you to a gynaecologist (a doctor who specialises in female reproductive health).
• If there's any concern that your cyst could be cancerous, your doctor will also arrange blood tests to look for high levels of chemicals that can indicate ovarian cancer.
• However, having high levels of these chemicals doesn't necessarily mean you have cancer, as high levels can also be caused by non-cancerous conditions such as:
• endometriosis
• a pelvic infection
• fibroids
• your period
• Whether an ovarian cyst needs to be treated will depend on:
• its size and appearance
• whether you have any symptoms
• whether you've been through the menopause
• In most cases, the cyst often disappears after a few months. A follow-up ultrasound scan may be used to confirm this.
• As post-menopausal women have a slightly higher risk of ovarian cancer, regular ultrasound scans and blood tests are usually recommended over the course of a year to monitor the cyst.
• Surgical treatment to remove the cysts may be needed if they're large, causing symptoms, or potentially cancerous.
• Ovarian cysts don't usually prevent you from getting pregnant, although they can sometimes make it harder to conceive.
• If you need an operation to remove your cysts, your surgeon will aim to preserve your fertility whenever possible. This may mean removing just the cyst and leaving the ovaries intact, or only removing one ovary.
• In some cases, surgery to remove both your ovaries may be necessary, in which case you'll no longer produce any eggs. Make sure you talk to your surgeon about the potential effects on your fertility before your operation.
There are various types of ovarian cysts, such as dermoid cysts and endometrioma cysts. However, functional cysts are the most common type. The two types of functional cysts include follicle and corpus luteum cysts.
• Follicle cyst
During a woman’s menstrual cycle, an egg grows in a sac called a follicle. This sac is located inside the ovaries. In most cases, this follicle or sac breaks open and releases an egg. But if the follicle doesn’t break open, the fluid inside the follicle can form a cyst on the ovary.
• Corpus luteum cysts
Follicle sacs typically dissolve after releasing an egg. But if the sac doesn’t dissolve and the opening of the follicle seals, additional fluid can develop inside the sac, and this accumulation of fluid causes a corpus luteum cyst.
• Other types of ovarian cysts include:
• dermoid cysts: sac-like growths on the ovaries that can contain hair, fat, and other tissue
• cystadenomas: noncancerous growths that can develop on the outer surface of the ovaries
• endometriomas: tissues that normally grow inside the uterus can develop outside the uterus and attach to the ovaries, resulting in a cyst
• Some women develop a condition called polycystic ovary syndrome. This condition means the ovaries contain a large number of small cysts. It can cause the ovaries to enlarge. If left untreated, polycystic ovaries can cause infertility.
Often times, ovarian cysts do not cause any symptoms. However, symptoms can appear as the cyst grows. Symptoms may include:
• abdominal bloating or swelling
• painful bowel movements
• pelvic pain before or during the menstrual cycle
• painful intercourse
• pain in the lower back or thighs
• breast tenderness
• nausea and vomiting
• Severe symptoms of an ovarian cyst that require immediate medical attention include:
• severe or sharp pelvic pain
• fever
• faintness or dizziness
• rapid breathing
• These symptoms can indicate a ruptured cyst or an ovarian torsion. Both complications can have serious consequences if not treated early.
• Most ovarian cysts are benign and naturally go away on their own without treatment. These cysts cause little, if any, symptoms. But in a rare case, doctor may detect a cancerous cystic ovarian mass during a routine examination.
• Ovarian torsion is another rare complication of ovarian cysts. This is when a large cyst causes an ovary to twist or move from its original position. Blood supply to the ovary is cut off, and if not treated, it can cause damage or death to the ovarian tissue. Although uncommon, ovarian torsion accounts for nearly 3 percent of emergency gynecologic surgeries.
• Ruptured cysts, which are also rare, can cause intense pain and internal bleeding. This complication increases your risk of an infection and can be life-threatening if left untreated.
• Your doctor can detect an ovarian cyst during a routine pelvic examination. They may notice swelling on one of your ovaries and order an ultrasound test to confirm the presence of a cyst. Ultrasound tests help determine the size, location, shape, and composition (solid or fluid filled) of a cyst.
• Imaging tools used to diagnose ovarian cysts include:
• ultrasound device: an imaging device used to visualize the ovary
• CT scan: a body imaging device used to create cross-sectional images of internal organs
• MRI: a test that uses magnetic fields to produce in-depth images of internal organs
• Because the majority of cysts disappear after a few weeks or months, doctor may not immediately recommend a treatment plan. Instead, they may repeat the ultrasound test in a few weeks or months to check your condition.
• If there aren’t any changes in your condition or if the cyst increases in size, doctor will request additional tests to determine other causes of your symptoms.
• These include:
• pregnancy test to make sure you’re not pregnant
• hormone level test to check for hormone-related issues, such as too much estrogen or progesterone
• CA-125 blood test to screen for ovarian cancer
We recommend treatment to shrink or remove the cyst if it doesn’t go away on its own or if it grows larger.
• Birth control pills
If you have recurrent ovarian cysts, we can prescribe oral contraceptives to stop ovulation and prevent the development of new cysts. Oral contraceptives can also reduce your risk of ovarian cancer. The risk of ovarian cancer is higher in postmenopausal women.
• Laparoscopy
If your cyst is small and results from an imaging test suggest to rule out cancer, doctor can perform a laparoscopy to surgically remove the cyst. The procedure involves doctor making a tiny incision near your navel and then inserting a camera laden small instrument into your abdomen to remove the cyst.
• Laparotomy
If you have a large cyst, doctor can surgically remove the cyst through a large incision in your abdomen. They’ll conduct an immediate biopsy, and if they determine that the cyst is cancerous, they may perform a hysterectomy to remove your ovaries and uterus