
Obstetrics relates to pregnancy, childbirth, and the post delivery period, as a medical specialty. Our services cover consultation on all complex pregnancy related conditions and treatment offered to women is quality and evidence based and has been sharply refined by the vast training and the world class international working experience

• Pre-pregnancy counseling is a consulting session conducted before you conceive.
• It helps in checking for possible risk factors during pregnancy and also gives a way to resolve any medical issues you may have before you become pregnant.
• Pre-pregnancy counseling and care will help you to become physically healthy and emotionally strong before you enter into the phase of pregnancy.
• You can discuss and clarify with us, all the things that concern you before you get pregnant, like starting prenatal vitamins, diet or any hereditary health issues. Many important points discussed include:
• Reproductive history: menstrual history, use of contraceptives, any previous sexually transmitted diseases.
• Medical and surgical history: Past health problems ,any past surgeries or hospitalizations should also be brought to the doctor’s notice.
• Current medications: any prescription, over-the- counter medications or herbal supplements that you may be currently taking.
• Weight: It is always better to have an ideal weight before you conceive. Gaining weight if you are underweight will reduce the risk of having a low birth-weight baby, and reducing weight if you are overweight will prevent the risk of high blood pressure during pregnancy.
• Workplace and home environment: potential hazards to conception or maintaining a pregnancy, such as exposure to lead or certain toxic solvents, radiation and cat feaces.
• Lifestyle: alcohol consumption, smoking and use of recreational drugs
• Exercise: Inform us about the type of exercises you perform or if you don’t exercise. Based on this, you may be advised to continue normal exercises during pregnancy until your doctor suggests otherwise.
• Diet: Having good dietary habits is beneficial during pregnancy. You will be advised to consume food rich in folic acid, calcium, fibre and other nutrients, and reduce the intake of caffeine, which is present in coffee, chocolates, soft drinks and medications, before getting pregnant.
• Family health history: Inform us about the presence of hereditary medical conditions and multiple births in the family.
• Prenatal vitamins: You should start taking folic acid supplements before you conceive, as folic acid reduces the chances of neural tube defects in your baby.
• Advice for older women: Women older than 35 years of age will be advised on the risks of infertility, abnormalities in the child and pregnancy complications, such as miscarriage and labour problems.
• We may also recommend:
1. Physical exam of your abdomen, heart, breasts, thyroid and lungs
2. Pap smear and pelvic examination
3. Lab tests to screen for hepatitis, HIV, rubella, syphilis and other conditions
4. Chart menstrual cycles to monitor ovulation and determine the most favorable time to get pregnant
5. Advise appropriate vaccinations against rubella .
6. Conduct genetic counseling for older mothers or those with a risk of hereditary diseases to help you understand the chances of birth defects or intellectual disability in the child.

• Prenatal care, also known as antenatal care, is a type of preventive healthcare. Its goal is to provide regular check-ups that allow doctors to treat and prevent potential health problems throughout the course of the pregnancy and to promote healthy lifestyles that benefit both mother and child.
• During check-ups, pregnant women receive medical information over
• maternal biological changes in pregnancy,
• prenatal nutrition including prenatal vitamins.
• Recommendations on management and healthy lifestyle changes,
• and prenatal screening and diagnosis,
• Proper care plays vital part in reducing the frequency of miscarriages, birth defects, low birth weight, neonatal infections and other preventable health problems.
• First visit in pregnancy:
• You can book an appointment as soon as you know that you're pregnant. It's best to consult as early as possible.
• During this first visit, we will take detailed history about your lifestyle, past illness, and health habits.
• Please inform us if
⇒ You've had any complications or infections in a previous pregnancy or delivery, such as pre-eclampsia or premature birth.
⇒ You're being treated for a chronic disease, such as diabetes or high blood pressure.
⇒ You or anyone in your family have previously had a baby with an abnormality.
⇒ There's a family history of an inherited disease.
• At first visit, you will be given information about:
⇒ Folic acid and vitamin D supplements
⇒ Nutrition, diet and food hygiene
⇒ Lifestyle modifications
Antenatal screening tests like Blood group and Rh status, CBC, urine test, sugar,syphilis, hepatitis B, HIV, rubella, Hb Electrophoresis and testing for thyroid disease.
• These tests will be discussed with you and you can choose whether you have them or not.
• a ultrasound for confirming number location and viability of embryo.
• Your next appointment should happen when you are 11-14 weeks pregnant. This is called the first antenatal visit or booking visit.
• Your due date is calculated by adding 40 weeks (280 days) to the first day of your last menstrual cycle. An ultrasound scan will give you a more accurate date for the birth of your baby.
• Between 11-13 weeks gestation you will be offered sonography called as early anamoly scan and blood test(Double Marker) which detects the Probable risk of Down's syndrome, Trisomy 18 and neural tube defects.
• Typically, routine checkups occur:
⇒ Once each month for weeks four through 28
⇒ Twice a month for weeks 28 through 36
⇒ Weekly for weeks 36 to birth
⇒ Women with high-risk pregnancies need to see their doctors more often.
⇒ Information about breast-feeding.
⇒ Information to prepare her for labour and birth (birth plan, pain relief options, how to recognize the onset of active labour).
⇒ Information about care of the new baby and preparations needed.
⇒ Information about routine procedures such as newborn screening and vitamin K prophylaxis.
⇒ Advice about postnatal self-care, along with information about postnatal depression and "baby blues".
• In early pregnancy transvaginal ultrasound will be performed at around 8 weeks to confirm viability, number and location of pregnancy.
• Second ultrasound is NT scan between 11 to 14 weeks. We call it as early anomaly scan and it will also confirm your due date.
• Third is an anomaly ultrasound between 18-20 weeks which is targeted to structural abnormalities so that a lethal anamoly ,if detected ,can be offered termination before 20 weeks of legal limit of termination of pregnancy.
• We could offer a growth scan or Dopplers at 28 to 34 weeks, if indicated.
• Additional ultrasounds are performed for other medical needs.
• Pregnancy Classes to educate about the pregnancy events and care , are scheduled monthly, usually on a saturday.
• Vaccination in pregnancy:
• We suggest one shot of Td vac at 20 weeks, Influenza vaccine at 26 weeks and single shot of Tdap(Combined vaccine for tetanus, diptheria and whooping cough) at 28 -30weeks.
⇒ Regular uterine contractions every 5 to 10 minutes for 1 hour.
⇒ Vaginal Bleeding. Spotting vaginally after an exam is normal. If any bleeding heavier than spotting go to the hospital.
⇒ frank gush of water from rupture of membranes.
⇒ Decrease fetal movement.

• Everyone expects pregnancy to bring an expanding waistline. But many women are surprised by the other body changes that pop up. Get the low-down on stretch marks, weight gain, heartburn and other "joys" of pregnancy. what you can do to feel better:
• As your uterus expands, you may feel aches and pains in the back, abdomen, groin area, and thighs.
• Many women also have backaches and aching near the pelvic bone due the pressure of the baby's head, increased weight, and loosening joints.
• Some pregnant women complain of pain that runs from the lower back, down the back of one leg, to the knee or foot. This is called sciatica. It is thought to occur when the uterus puts pressure on the sciatic nerve.what might help:
⇒ Lie down.
⇒ Rest.
⇒ Apply heat.
⇒ Call the doctor if pain does not get better
• A woman's breasts increase in size and fullness during pregnancy.
• As the due date approaches, hormone changes will cause your breasts to get even bigger to prepare for breastfeeding. Your breasts may feel full, heavy, or tender.
• In the third trimester, some pregnant women begin to leak colostrum from their breasts. Colostrum is the first milk that your breasts produce for the baby. It is a thick, yellowish fluid containing antibodies that protect newborns from infection.
What might help:
• Wear a maternity bra with good support.
• Put pads in bra to absorb leakage.
• Tell your doctor if you feel a lump or have nipple changes or discharge (that is not colostrum) or skin changes.
• Many pregnant women complain of constipation. Signs of constipation include having hard, dry stools; fewer than three bowel movements per week; and painful bowel movements.
• Higher levels of hormones due to pregnancy slow down digestion and relax muscles in the bowels leaving many women constipated. Plus, the pressure of the expanding uterus on the bowels can contribute to constipation.
What might help:
• Drink eight to 10 glasses of water daily.
• Don't drink caffeine.
• Eat fiber-rich foods, such as fresh or dried fruit, raw vegetables, and whole-grain cereals and breads.
• Try mild physical activity.
• Tell your doctor if constipation does not go away
• Many pregnant women complain of dizziness and lightheadedness throughout their pregnancies.
• Fainting is rare but does happen even in some healthy pregnant women. There are many reasons for these symptoms. The growth of more blood vessels in early pregnancy, the pressure of the expanding uterus on blood vessels, and the body's increased need for food all can make a pregnant woman feel lightheaded and dizzy.
What might help:
• Stand up slowly.
• Avoid standing for too long.
• Don't skip meals.
• Lie on your left side.
• Wear loose clothing.
• Call your doctor if you feel faint and have vaginal bleeding or abdominal pain.
• During your pregnancy, you might feel tired even after you've had a lot of sleep.
• Many women find they're exhausted in the first trimester. Don't worry, this is normal!
• This is your body's way of telling you that you need more rest. In the second trimester, tiredness is usually replaced with a feeling of well being and energy.
• But in the third trimester, exhaustion often sets in again. As you get larger, sleeping may become more difficult.
• The baby's movements, bathroom runs, and an increase in the body's metabolism might interrupt or disturb your sleep.
• Leg cramping can also interfere with a good night's sleep.
What might help:
• Lie on your left side.
• Use pillows for support, such as behind your back, tucked between your knees, and under your tummy.
• Practice good sleep habits, such as going to bed and getting up at the same time each day and using your bed only for sleep .
• Go to bed a little earlier.
• Nap if you are not able to get enough sleep at night.
• Drink needed fluids earlier in the day, so you can drink less in the hours before bed.
• Hormones and the pressure of the growing uterus cause indigestion and heartburn. Pregnancy hormones slow down the muscles of the digestive tract. So food tends to move more slowly and digestion is sluggish. This causes many pregnant women to feel bloated.
• Hormones also relax the valve that separates the esophagus from the stomach. This allows food and acids to come back up from the stomach to the esophagus. The food and acid causes the burning feeling of heartburn.
• As your baby gets bigger, the uterus pushes on the stomach making heartburn more common in later pregnancy.
What might help:
• Eat several small meals instead of three large meals — eat slowly.
• Drink fluids between meals — not with meals.
• Don't eat greasy and fried foods.
• Avoid citrus fruits or juices and spicy foods.
• Do not eat or drink within a few hours of bedtime.
• Do not lie down right after meals.
• Call your doctor if symptoms don't improve after trying these suggestions. Ask your doctor about using an antacid.
• Hemorrhoids are swollen and bulging veins in the rectum.
• They can cause itching, pain, and bleeding.
• Up to 50 percent of pregnant women get hemorrhoids. Hemorrhoids are common during pregnancy for many reasons.
• During pregnancy blood volume increases greatly, which can cause veins to enlarge. The expanding uterus also puts pressure on the veins in the rectum. Plus, constipation can worsen hemorrhoids.
• Hemorrhoids usually improve after delivery.
What might help:
• Drink lots of fluids.
• Eat fiber-rich foods, like whole grains, raw or cooked leafy green vegetables, and fruits.
• Try not to strain with bowel movements.
• About 20 percent of pregnant women feel itchy during pregnancy.
• Usually women feel itchy in the abdomen. But red, itchy palms and soles of the feet are also common complaints.
• Pregnancy hormones and stretching skin are probably to blame for most of your discomfort.
• Usually the itchy feeling goes away after delivery.
What might help:
• Use gentle soaps and moisturizing creams.
• Avoid hot showers and baths.
• Avoid itchy fabrics.
• Call your doctor if symptoms don't improve after a week of self-care.
At different times during your pregnancy, you might have sudden muscle spasms in your legs or feet. They usually occur at night. This is due to a change in the way your body processes calcium.
What might help:
• Gently stretch muscles.
• Get mild exercise.
• For sudden cramps, flex your foot forward.
• Eat calcium-rich foods.
• Ask your doctor about calcium supplements.
• In the first trimester hormone changes can cause nausea and vomiting. This is called "morning sickness," although it can occur at any time of day.
• Morning sickness usually tapers off by the second trimester.
What might help:
• Eat several small meals instead of three large meals to keep your stomach from being empty.
• Don't lie down after meals.
• Eat dry toast, saltines, or dry cereals before getting out of bed in the morning.
• Eat bland foods that are low in fat and easy to digest, such as cereal, rice, and bananas.
• Sip on water, weak tea, or clear soft drinks. Or eat ice chips.
• Avoid smells that upset your stomach.
• Call your doctor if you have flu-like symptoms, which may signal a more serious condition.
• Call your doctor if you have severe, constant nausea and/or vomiting several times every day.
Nosebleeds and nasal stuffiness are common during pregnancy. They are caused by the increased amount of blood in your body and hormones acting on the tissues of your nose.
What might help:
• Blow your nose gently.
• Drink fluids and use a cool mist humidifier.
• To stop a nosebleed, squeeze your nose between your thumb and forefinger for a few minutes.
• Call your doctor if nosebleeds are frequent and do not stop after a few minutes.
• Feelings of swelling, tingling, and numbness in fingers and hands, called carpal tunnel syndrome, can occur during pregnancy.
• These symptoms are due to swelling of tissues in the narrow passages in your wrists, and they should disappear after delivery.
What might help:
• Take frequent breaks to rest hands.
• Ask your doctor about fitting you for a splint to keep wrists straight.
• Stretch marks, skin changes
• Stretch marks are red, pink, or brown streaks on the skin. Most often they appear on the thighs, buttocks, abdomen, and breasts.
• These scars are caused by the stretching of the skin, and usually appear in the second half of pregnancy.
• Some women notice other skin changes during pregnancy. For many women, the nipples become darker and browner during pregnancy.
• Many pregnant women also develop a dark line (called the linea nigra) on the skin that runs from the belly button down to the pubic hairline.
• Patches of darker skin usually over the cheeks, forehead, nose, or upper lip also are common. Patches often match on both sides of the face. These spots are called melasma or chloasma and are more common in darker-skinned women.
What might help:
• Be patient — stretch marks and other changes usually fade after delivery.
Many women develop mild swelling in the face, hands, or ankles at some point in their pregnancies. As the due date approaches, swelling often becomes more noticeable.
What might help:
• Drink eight to 10 glasses of fluids daily.
• Don't drink caffeine or eat salty foods.
• Rest and elevate your feet.
• Call your doctor if your hands or feet swell suddenly or you rapidly gain weight — it may be preeclampsia.
• Temporary bladder control problems are common in pregnancy.
• Your unborn baby pushes down on the bladder, urethra, and pelvic floor muscles.
• This pressure can lead to more frequent need to urinate, as well as leaking of urine when sneezing, coughing, or laughing.
What might help:
• Take frequent bathroom breaks.
• Drink plenty of fluids to avoid dehydration.
• Do Kegel exercises to tone pelvic muscles.
• Consult your doctor if you experience burning along with frequency of urination — it may be an infection.
• During pregnancy, blood volume increases greatly. This can cause veins to enlarge.
• Plus, pressure on the large veins behind the uterus causes the blood to slow in its return to the heart.
• For these reasons, varicose veins in the legs and anus (hemorrhoids) are more common in pregnancy.
• Varicose veins look like swollen veins raised above the surface of the skin. They can be twisted or bulging and are dark purple or blue in color. They are found most often on the backs of the calves or on the inside of the leg.
What might help:
• Avoid tight knee-highs.
• Sit with your legs and feet raised.

• Down syndrome is caused by the presence of an extra chromosome number 21 in the cells of the developing baby.
• Down syndrome is always associated with mental retardation and is often associated with physical problems such as heart defects and difficulties with sight and hearing.
• It is not possible to assess the degree of handicap before the baby is born.
• About nine out of 10 babies with Down syndrome will survive their first year, and nearly half of these will reach 60 years of age.
• In an unscreened population, about one in every 700 babies is born with Down syndrome. Usually it is not inherited, so a baby can be affected even if there is no history of Down syndrome in the family.
• Although Down syndrome occurs more frequently as mothers get older, about 70 percent of babies with Down syndrome are born to women who are younger than 35 years old.
• The First Trimester Test is performed between 10 and 13 completed weeks of pregnancy to screen for Down syndrome.
• It combines information from an ultrasound examination of your baby with maternal blood analysis.
• It is suitable for women of all ages. It is a screening test and cannot determine definitely whether or not a baby has Down syndrome.
• The test identifies those women who have an increased risk of Down syndrome pregnancy so that they can be offered a diagnostic test (such as chorionic villus sampling). The diagnostic test identifies women who actually have an affected pregnancy.
• A sample of your blood is taken between 10 and 13 weeks of pregnancy.
• At the same time, an ultrasound scan is performed. Substances in your blood which are markers of Down syndrome and a specific ultrasound marker will be measured. The blood markers are pregnancy associated plasma protein A (PAPP-A) and human chorionic gonadotropin (free beta-hCG).
• The ultrasound marker is nuchal translucency (NT) thickness. In pregnancies with Down syndrome, PAPP-A tends to be low, and NT and HCG tend to be raised.
• The values of these markers are used together with your age to estimate the risk of having a pregnancy affected with Down syndrome.
• A risk is the chance of an event occurring. For example, a risk of Down syndrome of one in 100 means that if 100 women have this risk, we expect that one of these women will have a baby with Down syndrome and that 99 will not. This is the same as saying that the baby has a 1 percent chance of having Down syndrome and a 99 percent chance that it does not.
• A screen positive result means that you are in a high risk group for having a baby with Down syndrome.
• If you are in this group, you will be offered a diagnostic test.
• The result is screen positive if the risk of Down syndrome in the first trimester is one in 230 or greater.
• About one in every 20 women screened will be in this group. Most women with screen positive results do not have a pregnancy with Down syndrome. For example, of about 50 women with screen positive results for Down syndrome, only one would have an affected pregnancy.
• A screen positive result means that you are in a group with an increased risk of having a baby with an open neural tube defect.
• If the result is screen positive, you will be offered an ultrasound examination after 16 weeks of pregnancy, and possibly an amniocentesis.
• The result is screen positive when the AFP level is equal to or higher than two times the normal level for your stage of pregnancy.
• If the risk of Down syndrome based on the First Trimester Test is lower than one in 230, then the result is called screen negative, and a diagnostic test is usually not offered.
• If the risk of Down syndrome based on the Integrated Test is lower than one in 110, and the AFP level is less than two times the normal level for your stage of pregnancy, then the result is called screen negative, and a diagnostic test is usually not offered.
• Although a screen negative result means that your risk of having a baby with Down syndrome is not high, a screen negative result cannot rule out the possibility of a pregnancy with Down syndrome.
• No. About eight or nine out of 10 cases of Down syndrome are detected (classified as screen positive). This means that one or two out of 10 pregnancies with Down syndrome are missed (classified as screen negative). With the Integrated Test, about four out of five cases of spina bifida are detected, and one out of five is missed. Nearly all cases of anencephaly are detected.
• It is uncommon for a woman to have a baby with Down syndrome or an open neural tube defect, and it is even more uncommon for a woman with a screen negative result, but it does sometimes happen. This is because the screening test cannot completely distinguish affected from unaffected pregnancies. However small the risk is, the test cannot completely rule out the possibility of the baby having Down syndrome or open neural tube defect.
• Any woman may have a baby with Down syndrome, but the chance increases as a woman gets older.
• Therefore, we use age as one of the factors when assessing your risk of having a pregnancy with Down syndrome.
• It means that an older woman is more likely to have a result in the higher risk group (screen positive) and will therefore be offered a diagnostic test.
• For example, for women under the age of 35 about 4 percent will be screen positive, while in women who are 35 or older about 15 percent will be screen positive.
• Overall, about 5 percent of women will be screen positive, and about 85 percent of Down syndrome pregnancies will be identified with the First Trimester Test. Overall, about 1 percent of women will be screen positive with the Integrated Test.
• If the test is screen positive, you will be offered a diagnostic test, usually chorionic villus sampling (CVS) or possibly an amniocentesis.
• The diagnostic test will determine whether or not the pregnancy is actually affected.
• CVS is offered early in pregnancy (usually between 10 and 13 weeks). It involves taking a sample of placental tissue (using local anaesthetic) either by inserting a needle through your abdominal wall or by passing a fine instrument through the cervix.
• CVS is performed under the guidance of an ultrasound scan and does not involve a stay in the hospital. The CVS sample contains cells which can be used to tell whether or not the baby has Down syndrome.
• A result is usually ready within one to two weeks. There is a small risk associated with the CVS procedure. About 1 percent of women who have CVS will have a miscarriage as a result of the procedure.
• It depends on your particular result. If the test is screen positive for Down syndrome or at increased risk for trisomy 18 , an amniocentesis procedure will be offered, sometimes accompanied by a detailed ultrasound examination.
• If the test is screen positive for open neural tube defects, a targeted ultrasound examination is most commonly offered, although an amniocentesis is often suggested as well.
• An amniocentesis is a procedure in which the doctor obtains a small sample of fluid that surrounds the developing baby by passing a fine needle through the abdominal wall and into the uterus, under the guidance of an ultrasound scan.
• The sample is then sent for laboratory testing. This fluid sample can be used to diagnose chromosome problems like Down syndrome and trisomy 18.
• An amniocentesis is an invasive procedure, which means that there is a small risk of miscarriage (about one in 200) associated with it.
• Results of the test for Down syndrome and trisomy 18 usually take one to two weeks. A rapid technique for the diagnosis of Down syndrome and trisomy 18, fluorescence in situ hybridization (or FISH), is available at Women & Infants. FISH results usually take two days. Results for the test for open neural tube defects usually take five to seven days.
A genetic counselor will be available to discuss your baby's diagnosis in detail and options available to you. One option would be to continue the pregnancy and make arrangements for appropriate medical services at and after delivery. Placing the infant for adoption after birth can also be considered. Another option would be termination of pregnancy

A high-risk pregnancy is one that threatens the health or life of the mother or her fetus. It requires specialized care from specially trained providers.
Some pregnancies become high risk as they progress, while some women are at increased risk for complications even before they get pregnant for a variety of reasons.
Early and regular prenatal care helps many women have healthy pregnancies and deliveries without complications.
• Existing health conditions, such as high blood pressure, diabetes, or epilepsy, heart disease,or medical disease affecting baby.
• Overweight and obesity. Obesity increases the risk for high blood pressure, preeclampsia, gestational diabetes, stillbirth, neural tube defects, and cesarean delivery. Researchers have found that obesity can raise infants' risk of heart problems at birth by 15%.
• Multiple births. The risk of complications is higher in women carrying more than one fetus (twins and higher-order multiples). Common complications include preeclampsia, premature labor, and preterm birth. More than one-half of all twins and as many as 93% of triplets are born at less than 37 weeks' gestation.
• Other conditions include;
o recurrent miscarriages
o kidney disease
o cancer in pregnancy
o Rh blood factor problems
o history of pre-term birth or pregnancy complications
o genetic disease in the mother or family
o births birth defects identified before birth
• Any medical condition which develops during course of pregnancy and can potentially affect mother and baby need extra care.
• Women with high-risk pregnancies should receive care from a special team of health care providers to ensure the best possible outcomes.

• From conception to exclusive breast feeding (first 6 months) the baby completely depends on mother’s nutritional status.
• There is a considerable increase in the nutritional needs of the mother. On an average the pregnant women gains about 10 kg in pregnancy.
• Either low or excessive weight gain are harmful to the pregnant women and as well as the developing fetus (baby). A pregnant women need to consume about 350 extra calories per day, which translates to one additional meal.
• The growth and development of the baby is determined by the food taken by the mother. All the nutrients provided to the baby are derived from her food.
• A healthy diet during pregnancy should contain the right balance and combination of nutrients. If the mother is consuming a balanced diet comprising of various food groups, she gets the benefit of various nutrients that are necessary and increased during the pregnancy.
• It's a good idea to be as close as possible to the recommended weight for a given height (BMI) when trying for a baby as being overweight or underweight can affect babies’ growth and development. However consult a doctor before starting on any diet or exercise plan.
• A pregnant woman needs only 350 calories a day more than she did pre-pregnancy. An average size fruit provides 50 to 75 calories.
• Eat optimum food during pregnancy that includes whole grains, sprouted grams andØ fermented foods.
• Take Milk, Meat and Eggs in moderate quantitiesØ Eat recommended vegetables and fruits
• Take iron, Folate and calcium supplements regularly after 14-16 weeks of pregnancy andØ continue the same during lactation
• Avoid superstitions and food taboo
• Do not use alcohol and tobacco
• Wash fruits and vegetables to remove all traces of soil and pesticides. Thorough washing or soaking whole vegetables and fruits in salt water for 5 to 10 min, kills most bugs and removes pesticides substantially.
• Meat must be preserved separately and a separate chopping board must be used for meat.
• Wash all surfaces and utensils, and hands, after cleaning raw vegetables or meat – this will help to avoid food poisoning with bacteria or bacterial toxins (salmonella, staphylococcus, campylobacter or E.coli) and toxoplasmosis.
• Diet during lactation
• A balanced diet suitable for a nursing mother shall contain the same kind of food as those recommended during pregnancy, but slightly increased quantities.
• Twin factors of physical activity and active production of breast milk make additional demands for energy yielding foods, proteins and other nutrients.
• In general, most women who are breastfeeding need about 500 calories more than a woman who is non-pregnant and non- lactating; that is a total of 2,500 to 2,700 calories per day depending on her physical activity.
• Eating papaya causes abortion:
The truth is that raw papaya is suspected to contain chymopapaine which is supposed to induce abortion or early labor. But ripe papaya is considered to be safe. Moreover ripe papaya is a good source of vitamin A.
• Eating hot and spicy foods can cause abortion:
If eaten in moderation, it causes no harm to the baby. However, one should avoid very spicy food during pregnancy as many have the symptom of heartburn and very spicy food may increase it.

A normal vaginal delivery is the birth of a baby through the vagina when the pregnant woman goes into spontaneous labor at term i.e. between 37-42 weeks of gestation. Due date is calculated from the LMP or if periods are irregular, USG dating is done. It happens on its own without any help of drugs.
• The release of mucus plug. You may feel sticky, bloody discharge per vaginum
• Rupture of membranes. Bag of water ruptures causing gush of watery discharge
• Contractions- Strong pain felt at regular intervals in abdomen or back radiating to thighs with hardening of the uterus. Contractions push the baby in the birth canal.
Length of labour varies in women. First-time mothers have 12-24 hours of labour while later this may be reduced to 6-8 hours.
Three stages are there.
1. Stage 1- Onset of labour to full dilatation of cervix up to 10 cms.
• Early (latent phase)- Cervical dilatation from 0 to 3-4 cms.
• It lasts for 6-10 hrs in primigravida and shorter in multigravida.
• Contractions will be mild and irregular coming 10-30 minutes apart lasting 30-45 seconds.
• You can stay at home during this time and do relaxing activities like listening to music, watching TV, taking a warm bath or walk around.
• Active phase- from 4 cms to full dilatation 10 cms
• Labour is more intense lasting 3-6 hours.
• Contractions are more intense and frequent 3-5 minutes apart.
• Pain occurs in abdomen, back, and thighs and is difficult to bear.
• Epidural can be given at this stage.
• You should empty your bladder, drink fluids, breathe and relax.
• Sensation to bear down may occur, but do not bear down till doctor tells you to do so as pushing through undilated cervix is harmful.
2. Stage 2- Full dilatation to the delivery of the baby.
• Lasts for half to two hours.
• Contractions are very strong and close together, urge to bear down is strong.
• Nausea, vomiting, breathlessness, and fatigue occurs.
• Intense pain in vagina and perineum occurs when baby’s head comes out.
• You have to breathe and keep pushing hard.
3. Stage 3- Birth of placenta.
• From few minutes to half hour.
• Fatigue is full blown and you may relax now.
• Assisted or instrumental vaginal delivery
• Induced labour
• Caesarean section
This is a very vast topic but to summarise
• Prepare for natural birth throughout your pregnancy.
• You need a very strong body of labour.
• It’s just like preparation for a marathon.
• Without preparation, if you suddenly go for the marathon, you are sure to lose.
• In a similar fashion you cannot expect normal delivery without preparation.
• A uterus is a very strong muscle and needs to be well nourished for the stamina and pushing.
• Nutrition is very important.
• Physical preparedness- Exercise is not only for weight control, it is for physical and mental strength. Walk, yoga, kegel’s, squats need to be done on each single day. Control your breath, flexibility, relaxation etc.
• Birthing classes- They give you education and motivation for the intense labour you are about to experience.
• Choose the right doctor and hospital. You have to make a wise decision on your birthing options.
• Don’t gain too much weight. Labour is smooth and successful for women who gain correct and recommended amount of weight.
• Spouse support is very important.
• Mental strength also helps you, not only physical.
• Keep moving
• Keep breathing
The art of normal delivery is disappearing each day due to various reasons but still with all the information you can experience it in expert hands. You, your family, your doctor, hospital, physical and mental strength, baby characteristics all play a role to facilitate a normal delivery. So make your options clear and work towards the same nevertheless if due to some unavoidable reason you land up in a operative delivery you should not feel sad as nowadays both routes are safe and our main aim is a healthy mother and baby.

• Labour and childbirth is usually a painful experience and women vary in their response to it.
• Some women are keen to avoid drugs or other medical interventions while others are happy to consider all available options.
• For a woman having her first baby, the experience of labour (and her reaction to it) is unpredictable.
• For this reason, it is a good idea to be aware of the options for pain relief that are available and to know something about the different methods.
• You may have a plan for how you hope to manage your labour, but it is best to be prepared to be flexible.
• Research suggests that adequate preparation can help to reduce pain or at least modify the perception of pain and reduce anxiety, which can help you to better cope with labour. There are several non-drug pain relief options:
• Being in good physical condition is important. Exercise gently and regularly throughout your pregnancy, avoid cigarettes and alcohol, and eat a healthy, balanced diet.
• Knowing what to expect during the various stages of labour can help reduce anxiety. Antenatal classes are strongly recommended.
• Breathing techniques may help you to ‘ride the waves’ of each contraction.
• Using distractions like music can help to take your mind off the pain.
• Hot or cold packs, massage, a warm shower or immersion in a warm bath, and keeping active may all be helpful.
• Epidural injections are the most effective pain relief available.
• They are used for vaginal births and also for caesarean sections, because they allow the mother to stay awake and alert during the baby’s birth.
• Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
• Possible side effects and complications of epidural anaesthesia include:
• The anaesthesia may not be complete and you may still experience some pain. This may require the procedure to be repeated.
• After the epidural has been inserted, your blood pressure may drop, causing you to feel faint and nauseated. This may also cause stress to your baby. This is treated by giving intravenous fluid.
• An epidural often causes some muscle weakness in the legs, so women who have had an epidural anaesthetic may be confined to bed.
• The lack of sensation in the lower body means that you will not be able to tell when you need to urinate. A urinary catheter will be inserted in most cases.
• Epidurals can lengthen the second stage of labour.
• The likelihood of having a normal vaginal delivery is reduced.
• If you are unable to push effectively, due to altered sensation and reduced muscle strength, the baby may have to be delivered by forceps or vacuum cup.
• Around one per cent of women experience headache immediately following the procedure.
• Some women experience itchiness after having an epidural. This can usually be effectively treated using antihistamines.
• Some women experience pain or tenderness where the epidural was injected.

Pregnancy ends with delivery which can be either vaginal delivery/ assisted vaginal delivery in the form of forceps/ ventouse or a caesarean section.
Each type of delivery has its own pros and cons – risks and benefits.
Sometimes for the sake of mother or the baby or because of certain medical conditions you need go for caesarean delivery.
These days the technique is such that it is very safe in good hands.
Nevertheless since it’s a major operation in which we are opening the abdomen , some complications may arise.
• Pain: This may sometimes take some while to subside and one may have to pain killers for some time.
• Infection: Infection of wound/womb/catheter induced urinary tract infection:
• Bleeding : Bleeding is a bit more in a caesarean section than a vaginal birth.
• Adhesions: Sometimes there is a tendency of the intestines /urinary bladder to stick to the operation site and this can lead to pain / difficulty in next operation .
• Serious issues : Serious complications like injury to intestines/ urinary system/requirement for another operation/ excessive bleeding requiring removal of the uterus are very rare.
• Anaesthesia Complications: Risks associated with the type of anaesthesia are also there. Most common is a spinal headache which may occur when anaesthesia is given in the spine.
• Breathing issues in babies : Sometimes the babies born without start of labour through caesarean may have transient breathing problems.
Having one caesarean there is a risk of having another caesarean although after the first one there are still chances of a vaginal birth(VBAC).
• An emergency caesarean is many a times better than a traumatic vaginal delivery by forces/ ventouse. There is a decreased risk of birth injuries or birth asphyxia in the newborn (mental retardation due to lack of oxygen)
• C Sections can save the life of your baby : Caesarean can save the life of the baby in certain circumstances like breech/ transverse lie and other abnormal presentations.
• When the baby passes meconium in early labour or it has fetal distress caesarean remains the only option in order to avoid future serious repercussions/ death of the baby.
• C sections can help in difficult medical situations: In cases where the baby gets stuck in the pelvis in a labouring patient sometimes the uterus gets ruptured and this leads to loss of the baby within minutes and death of the mother if not managed in time by a caesarean.
Although the term caesarean may seem intimidating but thousands are being done safely for maternal/ fetal and medical indications leading to happy mothers and healthy babies!

A postpartum (or postnatal) period begins immediately after the birth of a child and extends for about six weeks, as the mother's body, including hormone levels and uterus size, returns to a non-pregnant state.
• You need special care for your body after giving birth to regain the energy and strength..
• Lots of things like lack of sleep, taking care of baby, anxiety over baby’s health, hormonal changes, wondering and worrying about your body shape, other physical discomforts like vaginal discharge, cramps etc. may affect you during this post-partum period.
• The post-partum period is usually six to eight weeks from the day of your delivery.
• This period is considered as a highly sensitive period and all the post- partum care systems as per the Indian culture, place a great emphasis on encouraging fast healing, boosting immunity, and improving the production of milk.
• A typical episiotomy or second-degree tear involves skin and muscle. These usually require stitches and heal in two to three weeks. (The stitches dissolve on their own during this time.) Some women feel little pain after a week, while others have discomfort for a month
• Healing times vary, but in general, the deeper the cut or tear, the longer the recovery time. A small, or first-degree, tear involves the skin only (not muscle), and stitches may not even be necessary. These tears generally heal quickly with little discomfort.
• A typical episiotomy or second-degree tear involves skin and muscle. These usually require stitches and heal in two to three weeks. (The stitches dissolve on their own during this time.) Some women feel little pain after a week, while others have discomfort for a month.
• We will give you detailed instructions on how to care for yourself. It may help to:
• Apply an ice pack with a soft covering to your perineum right after you give birth to reduce swelling and discomfort. Ask for a new ice pack every few hours over the next 12 hours or so.
• Take ibuprofen or acetaminophen for pain relief. (Don't take aspirin if you're breastfeeding.) If you have an extensive tear, you may need prescription pain medication.
• Change your sanitary pad every time you use the bathroom.
• Use a squirt bottle to pour warm water on your perineum while you're urinating. The water dilutes your urine so it doesn't burn as much when it comes in contact with your skin. Cleanse the area with another squirt afterward.
• Pat yourself dry from front to back to avoid introducing germs from the rectum into the vaginal area.
• Don't sit for long periods of time while your perineum is still very sore.
• Start taking warm soaks or sitz baths 24 hours after you give birth. Do this for 20 minutes, three times a day.
• For a sitz bath, you fill a shallow plastic tub with warm water and sit on it, with your perineum in the water. This way, you can soak your perineal area several times a day. Most hospitals will provide you with a sitz bath basin, and they're also available at most drugstores.
• Start doing Kegel exercises the day you give birth. These help restore muscle tone, stimulate circulation, and speed healing. (Contracting your pelvic floor muscles supports the wound so you'll feel less of a pulling sensation on your stitches when you move.)
• Get plenty of rest, and don't take on any unnecessary chores. Save your energy for taking care of your baby and yourself so your body can heal.
• After a caesarean section, you may experience pain at the surgical site and have to stay 2 to 3 days in the hospital.
• The medications administered for a C-section may make you feel nauseous or itchy and the surgical site may hurt while you nurse your baby. Ask for help if you find it difficult to nurse
• Your blood pressure, bleeding and heart rate will be monitored regularly. The size of your uterus and firmness will be checked
• Your doctor will prescribe medications to relieve pain
• Try sitting up and moving around several times a day to promote healing
• Bowel movements are painful after childbirth so it is important to include a high fiber diet or stool softeners to soften the stools and allow easier passage
• You may experience skin changes and hair loss due to hormonal changes. This is normal and will get better after a few months
• It is important for your baby to continue to breastfeed; seek help if you experience discomfort, breast soreness or infection
• You may feel sad and depressed post-delivery. This is called ‘postpartum depression’ and can be very serious, impacting your ability to care for your new baby. Seek help if you are unable to care for yourself or the baby as treatment is available to make you feel better
• Inform your doctor if you experience deep vein thrombosis or blood clots in the legs
• You should exercise regularly as instructed by your doctor to help healing, improve mood and to regain your pre-pregnancy body weight’
• Around one in 550 women experience ongoing patches of numbness on the back near the injection site.
• Very rare complications include infection, blood clots and difficulty breathing.

Breast milk provides the ideal nutrition for infants.
It has a nearly perfect mix of vitamins, protein, and fat -- everything your baby needs to grow.
And it's all provided in a form more easily digested than infant formula.
Breast milk contains antibodies that help your baby fight off viruses and bacteria. Breastfeeding lowers your baby's risk of having asthma or allergies. Plus, babies who are breastfed exclusively for the first 6 months, without any formula, have fewer ear infections, respiratory illnesses, and bouts of diarrhea.
They also have fewer hospitalizations and trips to the doctor.
Breastfeeding has been linked to higher IQ scores in later childhood in some studies. What's more, the physical closeness, skin-to- skin touching, and eye contact all help your baby bond with you and feel secure.
Breastfed infants are more likely to gain the right amount of weight as they grow rather than become overweight children.. It's been thought to lower the risk of diabetes, obesity, and certain cancers as well, but more research is needed.
Breastfeeding burns extra calories, so it can help you lose weight faster.
It releases the hormone oxytocin, which helps your uterus return to its pre- pregnancy size and may reduce uterine bleeding after birth.
Breastfeeding also lowers your risk of breast and ovarian cancer.
It may lower your risk of osteoporosis, too.
Since you don't have to buy and measure formula, sterilize nipples, or warm bottles, it saves you time and money.
It also gives you regular time to relax quietly with your newborn as you bond.
The first few days after birth, your breasts make ideal "first milk." It's called colostrum.
Colostrum is thick, yellowish, and scant, but there's plenty to meet your baby's nutritional needs.
Colostrum helps a newborn's digestive tract develop and prepare itself to digest breast milk.
Most babies lose a small amount of weight in the first 3 to 5 days after birth. This is unrelated to breastfeeding.
As your baby needs more milk and nurses more, your breasts respond by making more milk.
Experts recommend breastfeeding exclusively (no formula, juice, or water) for 6 months.
If you supplement with formula, your breasts might make less milk.
Even if you breastfeed less than the recommended 6 months, it's better to breastfeed for a short time than no time at all.
You can add solid food at 6 months but also continue to breastfeed if you want to keep producing milk.
You'll know your baby is "latched on" correctly when both lips are pursed outward around your nipple. Your infant should have all of your nipple and most of the areola, which is the darker skin around your nipple, in his mouth.
• A = Awareness. Watch for your baby's signs of hunger, and breastfeed whenever your baby is hungry. This is called "on demand" feeding. The first few weeks, you may be nursing eight to 12 times every 24 hours.Hungry infants move their hands toward their mouths, make sucking noises or mouth movements, or move toward your breast. Don't wait for your baby to cry. That's a sign he's too hungry.
• B = Be patient. Breastfeed as long as your baby wants to nurse each time. Don't hurry your infant through feedings. Infants typically breastfeed for 10 to 20 minutes on each breast.
• C = Comfort. This is key. Relax while breastfeeding, and your milk is more likely to "let down" and flow. Get yourself comfortable with pillows as needed to support your arms, head, and neck, and a footrest to support your feet and legs before you begin to breastfeed.
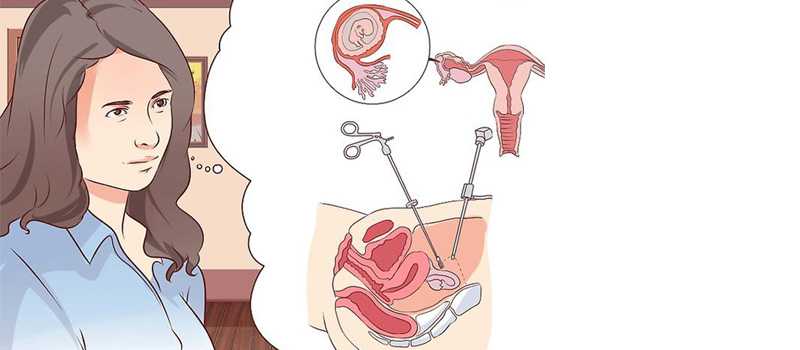
An ectopic pregnancy occurs when the fertilized egg attaches itself in a place other than inside the uterus. The fallopian tubes are not designed to hold a growing embryo; thus, the fertilized egg in a tubal pregnancy cannot develop properly and must be treated. An ectopic pregnancy happens in 1 out of 50 pregnancies.
Unfortunately, the baby cannot be saved in an ectopic pregnancy. Treatment is usually needed to remove the pregnancy before it grows too large.
The main treatment options are:
• expectant management – your condition is carefully monitored to see whether treatment is necessary
• medication – a medicine called methotrexate is used to stop the pregnancy growing
• surgery – surgery is used to remove the pregnancy, usually along with the affected fallopian tube
If you have no symptoms or mild symptoms and the pregnancy is very small or can't be found, you may only need to be closely monitored, as there's a good chance the pregnancy will dissolve by itself.
This is known as expectant management.
The following is likely to happen:
• You'll have regular blood tests to check that the level of hCG in your blood is going down – these will be needed until the hormone is no longer found.
• You may need further treatment if your hormone level doesn't go down or it increases.
• You'll usually have some vaginal bleeding – use sanitary pads or towels, rather than tampons, until this clears up.
• You may experience some tummy pain – take paracetamol to relieve this.
• You'll be told what to do if you develop more severe symptoms.
The main advantage of monitoring is that you won't experience any side effects of treatment.
A disadvantage is that there's still a small risk of your fallopian tubes splitting open (rupturing) and you may eventually need treatment.
If an ectopic pregnancy is diagnosed early and is eligible under defined medical criteria, treatment with a medicine called methotrexate may be recommended.
This works by stopping the pregnancy from growing. It's given as a single injection into your buttocks.
You may need to stay in hospital after treatment, and regular blood tests will be carried out to check if the treatment is working.
A second dose is sometimes needed and surgery may be necessary if it doesn't work.
You need to use reliable contraception for at least 3 months after treatment.
This is because methotrexate can be harmful for a baby if you become pregnant during this time.
It's also important to avoid alcohol until you're told it's safe, as drinking soon after receiving a dose of methotrexate can damage your liver.
Other side effects of methotrexate include:
• tummy pain – this is usually mild and should pass within a day or two
• dizziness
• feeling and being sick
• diarrhoea
There's also a chance of your fallopian tubes rupturing after treatment. You'll be told what to look out for and what to do if you think this has happened.
In most cases, keyhole surgery (laparoscopy) will be carried out to remove the pregnancy before it becomes too large.
During a laparoscopy:
• you're given general anaesthetic, so you're asleep while it's carried out
• small cuts (incisions) are made in your tummy
• a thin viewing tube (laparoscope) and small surgical instruments are inserted through the incisions
• the entire fallopian tube containing the pregnancy is removed if your other fallopian tube looks healthy – otherwise, removing the pregnancy without removing the whole tube may be attempted (salphingostomy)
Removing the affected fallopian tube is the most effective treatment and isn't thought to reduce your chances of becoming pregnant again.
Your doctor will discuss this with you beforehand, and you'll be asked whether you consent to having the tube removed.
Most women can leave hospital a few days after surgery, although it can take 4 to 6 weeks to fully recover.
If your fallopian tube has already ruptured, you'll need emergency surgery.
The surgeon will make a larger incision in your tummy (laparotomy) to stop the bleeding and repair your fallopian tube, if that's possible.

• Miscarriage of a pregnancy is a physically and emotionally challenging ordeal. When pregnancy loss is repetitive, these feelings are magnified.
• While the risk of miscarriage increases with increasing maternal age, overall approximately 13% of all recognized first pregnancies miscarry.
• The risk of a second consecutive miscarriage is only slightly increased to 17%. However, the risk of miscarriage after two consecutive pregnancy losses rises to 35 to 40% and continues to rise with each subsequent miscarriage.
• It is estimated that between 2 to 5% of couples desiring pregnancy will suffer from recurrent pregnancy loss
The most common causes of recurrent miscarriages are as follows:
• Genetic causes
• Immunologic causes
• Anatomic causes
o Uterine septum (the anomaly most commonly associated with pregnancy loss)
o Bicornuate uterus
≈ Incompetent cervix
≈ Uterine polyps or fibriods
• Infectious causes
• Environmental causes
o Smoking
o Excessive alcohol consumption
o Caffeine
• Endocrine factors
o Diabetes mellitus
o Antithyroid antibodies
• Hematologic disorders

MTP is Medical Termination of Pregnancy. MTP should always be performed by a registered specialist at a place recognized by government authorities.
• Failure of contraception.
• Possible hazards on physical/mental health of the mother.
• Pregnancy caused by rape.
• Possible hazard to the health of growing fetus.
Medical Termination of Pregnancy is legally permitted up to 20 weeks of gestation. Pregnancy termination performed in first trimester is safer than in second trimester since it has fewer complications.
It is illegal to perform MTP after determining sex of the child as Government of India has banned sex determination.
Medication and surgical (uterine dilation and suction aspiration) abortion are both safe and effective approaches for appropriately selected patients. The choice is based upon availability, gestational age, and patient preference. Women seeking abortion care should be counselled about the advantages and disadvantages of both options.
A medical abortion is a type of non-surgical abortion in which medication is used to bring about abortion. An oral preparation for medical abortion is commonly referred to as an abortion pill .As per the law, it can be prescribed upto 7 weeks of pregnancy.
Medical abortion
• Haemorrhage
• Incomplete abortion
• Uterine or pelvic infection
• Ongoing intrauterine pregnancy, requiring a surgical abortion for completion
• Misdiagnosed/unrecognized ectopic pregnancy
First-trimester surgical abortion is effective in terminating pregnancy in 98 to 99 percent of procedures and has a complication rate of 0 to 3 percent . The major complications of surgical abortion are incomplete evacuation, uterine perforation, problems related to anesthesia, and endometritis.
It is often advised to contact a health care provider if there is bleeding to such degree that more than two pads are soaked per hour for two consecutive hours.

Choosing the birth control method that is optimal for you will depend on a lot of factors that include your age, life style and needs. Are you just trying to postpone pregnancy, spacing between children or have you already ‘completed’ your family?
o Effectiveness: Most reversible types of birth control are not 100% effective, but some are more effective than others. If a pregnancy is not possible for you, you would want to choose a method with a very high effectiveness rate. On the other hand, if pregnancy is an option for you, a method that is not as effective may not be such a bad thing.
o Effort: Consider how much effort you are willing to put into your birth control. Is it something you want to think about every time you have sex? Every day? Every couple weeks? Every couple years?
o Reversibility: If you think you may want to have children soon, you don't want to choose a method that is not quickly or easily reversible: i.e. hormonal methods and surgical procedures.
o Cost: Some methods are cheaper than others.
o Protection: If you are in a long-term relationship and do not need protection from STDs or STIs, then you may choose to not use condoms. But condoms are the only form of contraception that also prevents the transmission of HIV and other STDs.
o Prior experience/side effects: One method may not have worked well for you in the past, so you do not want to choose a similar method to that one. For example, hormonal birth control may have caused side effects for you, and you may want to look into other methods with less side effects.
1 -Barrier methods: Diaphragms, cervical caps, male condoms, female condoms, and sponges. These methods are often used with spermicide and create a physical barrier against sperm so they cannot enter the uterus. Overall, these methods are generally cheaper and have fewer side effects, but they do have a lower pregnancy prevention rate.
2-Hormonal methods: IUDs, shots (Depoprovera), patches, vaginal ring (Nuva Ring), and the pill. These methods regulate hormones in the female body (estrogen and progestin) in order to prevent pregnancies. Pills are usually taken every day; rings, shots, and patches every few weeks; and IUD's and implants every couple of years. They are very effective, but may cause serious side effects.
3-Intra uterine device: The copper IUD does not use hormones, but it also has side effects to be considered.
4-All natural methods: withdrawal and Feminine Awareness Method (FAM).
These methods have no side effects and are free. However, the withdrawal method (removing the penis before ejaculation) requires a large amount of trust and experience, and may be ineffective. Natural methods are most successfully used with another form of birth control.
5-Permanent methods: vasectomy and tubal ligation. These procedures are for couples that no longer want to have children and are 100% effective. However tubal ligation is not reversible. Most couples choose to get a vasectomy, because it is a quick, fairly painless, and cheaper procedure.
6-Emergency procedures: Plan B. Plan B is a pill that can be taken, up to five days after failure of birth control or unprotected sex, to reduce the risk of a pregnancy occurring.
It uses a large dose of hormones to have this effect and is disruptive to a woman's cycle; it's an emergency procedure that is not intended for everyday birth control.