Some of the disorders that may be treated with a hysterectomy are:
• Constant heavy bleeding that has not been controlled by medicines or dilatation and curettage (D&C)
• Endometriosis that causes pain or bleeding and does not respond to other treatments
• Chronic pelvic pain
• Prolapse uterus - a fallen (sagging) uterus
• Precancerous or cancerous cells or tissue present in the uterus
• Tumours in the uterus.
Vaginal hysterectomy is a surgical procedure to remove the uterus through the vagina.
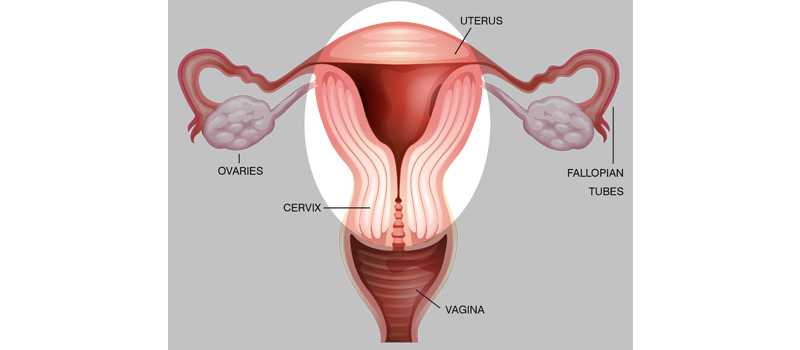
During a vaginal hysterectomy, the surgeon detaches the uterus from the ovaries, fallopian tubes and upper vagina, as well as from the blood vessels and connective tissue that support it. The uterus is then removed through the vagina. Other ways in which the uterus may be removed are:
• Abdominal Hysterectomy - Having the uterus removed through an incision in your lower abdomen.
• Laparoscopic Hysterectomy through key hole incisions made in the abdomen
• Doctor will have choice for the method of hysterectomy that is appropriate for your medical condition.
The IV and catheter are removed 1 or 2 days after the surgery. You may stay
in the hospital about 3 to 5 days.
After you go home, get plenty of rest. Do not do any heavy lifting or otherwise
strain the abdomen muscles for 4 to 6 weeks.
Follow your consultant's instructions for dealing with pain and preventing
constipation.
If you were having menstrual periods before the surgery, you will no longer
have them after the operation. You also cannot become pregnant. If your ovaries were removed, menopause starts right away and your doctor may prescribe hormone therapy. Be sure to discuss any concerns you have about
these effects and treatment with your doctor before the surgery.
After-effects of general anesthesia
Most modern anaesthetics are short lasting. You should not suffer from any after-effects for more than a day after your surgery. During the first 24 hours you may feel more sleepy than usual and your judgement may be impaired.
Catheter
You may have a catheter in your bladder to allow drainage of your urine. This is usually for up to 24 hours after your operation until you are easily able to walk to the toilet to empty your bladder. If you have difficulties passing urine, you may need to have a catheter for a few more days.
Scars
A Vaginal Hysterectomy is performed through your vagina so the scar will be out of sight. However, if you have keyhole surgery as part of your operation, you will have between two and four small scars on different parts of your abdomen. The scar will be anywhere between 0.5 cm and 1 cm long.
Stitches and dressings
Removal of the stitches in your vagina is not required as they are dissolvable. You may notice a stitch, or part of a stitch, coming away after a few days or maybe after a few weeks. This is normal and nothing to worry about. If you have keyhole surgery, your cuts may be closed by stitches or glue. Glue and some stitches dissolve by themselves. Other stitches may need to be removed, you will be given information about this. Your cuts will initially be covered with a dressing.
Packs
You may have a pack in your vagina after the surgery to reduce the risk of bleeding. A nurse will remove this after your operation while you are still in the hospital.
Vaginal bleeding
You can anticipate having some vaginal bleeding for one to two weeks after your procedure. This is like a light period and is red or brown in colour. Some women have slight or no bleeding initially, and then have a sudden flow of old blood or fluid about 10 days later. This usually stops quickly. You should use sanitary towels rather than tampons as using tampons could rise the risk of infection.
Pain and discomfort
You can expect pain and uneasiness in your lower abdomen for the first few days after your surgery. When leaving hospital, you will be provided with painkillers for the pain you are undergoing.
Trapped wind
Post-surgery your bowel may slow down for the time being, causing air or 'wind' to be trapped. This can cause some discomfort until it is passed. Getting out of bed and walking around will help. Once your bowels start to move, the trapped wind will ease.
Starting to eat and drink
After the surgery, you may have a drip in your arm to provide fluids. When you are able to drink again, the drip will be removed. You will be offered water or cup of tea and something light to eat.
Formation of blood clots - how to reduce the risk
There is a small possibility of formation of blood clots in the veins in your legs and pelvis (deep vein thrombosis) after any surgery. These clots can travel to the lungs (pulmonary embolism), which could be fatal. You can reduce the risk of clots by:
• Start walking/moving about as soon as you can after your operation.
• Perform exercises while you are resting, for example: pump each foot up and down briskly for 30 seconds by moving your ankle or move each foot in a circular motion for 30 seconds and bend and straighten your legs - one leg at a time, three times for each leg.
You may also advised other methods to reduce the risk of a clot formation, particularly if you are overweight or have other health issues.
Physiotherapy
You will be given guidance and information about exercises to help you recover fast and ways to gain mobility without difficulty.
Tiredness and feeling emotional
A hysterectomy can also be emotionally traumatic and many women during this stage feel tearful and emotional.
Recovery from a hysterectomy if can be longer if:
• You had health complications before your operation; for example, women with diabetes may heal at a slower pace and may be more prone to infection.
• You are overweight - Patients can take a longer duration to recuperate from the effects of the anaesthetic and there is also a higher risk of complications such as infection and thrombosis.
• There were any other complications during your surgery.
Get in touch with the hospital and your medical team:
• You develop a fever over 100 degree F
• You have nausea and vomiting
• You have chest pain or become short of breath
• You have bleeding from the vagina
• You have leakage from the incision or the incision opens up
• You have pain where you urinate
• You have swelling, redness or pain in your leg
Your own recovery will depend on:
• How fit you are before your operation
• The reason you are having a hysterectomy
• The exact type of hysterectomy that you have
• How smoothly the surgery goes and whether there are any complications.
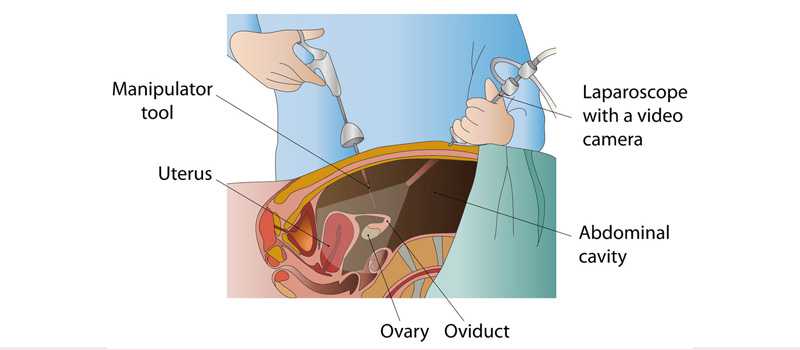
Laparoscopy, also known as key hole surgery, is a surgical procedure used to
examine the organs inside the abdomen. It’s a low-risk, minimally invasive
procedure that requires only small incisions.
Laparoscopy uses an instrument called a laparoscope to look at the
abdominal organs. A laparoscope is a long, thin tube with a high-intensity light
and a high-resolution camera at the front. The instrument is inserted through
an incision in the abdominal wall. As it moves along, the camera sends
images to a video monitor.
Laparoscopy allows surgeon to see inside abdomen in real time, without open
surgery.
Working this way has several advantages compared with traditional surgery. Because it involves less cutting:
• You have smaller scars.
• You get discharge quicker.
• You'll feel less pain while the scars heal, and they heal quicker.
• You get back to your normal activities sooner.
• You may have less internal scarring.
With traditional methods, you might spend 4 days or more in the hospital for open surgery, and your total recovery might take 4 to 8 weeks. If you have laparoscopic surgery, you might stay only 2 nights in the hospital and recover in 2 or 3 weeks.
Common procedures performed are:
1- DIAGNOSTIC LAPAROSCOPY
2- Laparoscopic adhesiolysis
3- Endometriosis fulguration
4-Myomectomy (fibroid removal)
5- Tubal ligation (TT)
6-Ovarian drilling for PCOS
7- Twisted ovarian cyst
8-Ovarian cyst removal
9-Tubal ligation
10- Tubal ectopic surgery
11- Tubo-ovarian masses
Tubal ligation is surgery to close a woman's fallopian tubes. (It is sometimes called "tying the tubes.") The fallopian tubes connect the ovaries to the uterus. A woman who has this surgery can no longer get pregnant.
Description
Tubal ligation is done in a hospital through an incision in abdomen or
laparoscopically.
The procedure takes about 30 minutes.
• Surgeon will make 1 or 2 small surgical cuts in your belly. Most often, they are around the belly button. Gas may be pumped into your belly to expand it. This helps your surgeon see your uterus and fallopian tubes.
• A narrow tube with a tiny camera on the end (laparoscope) is inserted into your belly. Instruments to block off your tubes will be inserted through the laparoscope or through a separate small cut.
• The tubes are either burned shut (cauterized) or clamped off with a small clip
or ring (band).
Tubal ligation can also be done right after you have a baby through a small
cut in the navel. It can also be done during a C-section.
Tubal Ligation, or tying of the tubes as it is more commonly referred to, is the most popular form of birth control the world over, and involves closing or blocking the fallopian tubes. However, you could have a change of heart later. In such a situation, you would need a Tubal Recanalisation / Reversal procedure to unblock your fallopian tube for passage of the sperm and the ovum.
What happens during the procedure?
A Tubal Recanalisation is done via laparoscopy or laparotomy to minimise risk of injury. During the procedure, the specialist places a speculum in the vagina and passes a catheter through the cervix into the uterus. The block is identified using a laparoscope or using a liquid contrast agent that is injected through the catheter. Once the block is identified, it is removed using a small catheter that is threaded through the previous catheter.
You could have minimal bleeding for a few days after the recanalisation procedure. However, of you experience pain, cramps, fever or abnormal discharge, see our specialist immediately.
Although microsurgical reversal completely reverses the tubal ligation, other factors such as duration of sterilisation, the technique used, and the length of the tube that remains after the reversal come in to play in deciding pregnancy rate.
The surgical removal of fibroids, which are tumours that grown within the muscle of the uterus, is called Myomectomy. The tumours can vary in size and number, and maybe the cause of long standing infertility or miscarriages, depending on their location. The procedure removes the tumours safely and improves chances of pregnancy.
we offer Hysteroscopic Myomectomy, Laparoscopic Myomectomy and Laparotomy-Abdominal Myomectomy depending on the number of fibroids to be removed, their location and size.
What happens during the procedure?
During a Hysteroscopic Myomectomy, we remove the fibroids through the
cervix. Although it is done under general anaesthesia, no incision is made.
You will be given a course of estrogen after the surgery to promote regrowth
of the uterine lining. Recommended Hospital Stay: Half a day and Recovery
time: 5-6 days.
In a Laparoscopic Myomectomy, the tumours are removed through a tiny
incision, under general anaesthesia. The recommended hospital stay is 1-2
days and recovery time is about 1 -2 weeks.
An Abdominal Myomectomy is an open surgery where the fibroids are
removed via an incision in the abdomen, through a laparotomy. We recommend this method when you have multiple fibroids that are larger than 10cms. The surgery, which is performed under general anaesthesia, takes
about 2 hours. The recommended hospital stay is 3 - 4 days and the recovery
time is about 4-6 weeks.
Ovarian cysts are fluid filled growths of the ovaries and can occur across all
age groups.
There are three kinds of cysts: functional, neoplastic – which may or may not
be cancerous, and endometriotic. While most ovarian cysts are non-
cancerous, they can be a contributing factor of infertility and also bring down
the quality of the eggs.
An Ovarian Cystectomy is the surgical removal of ovarian cysts, while
preserving the ovary.
What happens during the procedure?
The procedure is performed through laparoscopy (keyhole) or laparotomy (larger abdominal incision), under anaesthesia. The latter is often recommended when there is a suspicion of cancer, as it offers the specialist a good view of the abdominal and pelvic organs.
If the cysts are non cancerous, they are carefully removed, leaving the ovary
intact. However, if cancer is found, one or both the ovaries may be removed.
After the Laparoscopy procedure, you would need to avoid strenuous activity
for atleast a week. If you have had a laparotomy, you would need to remain in
hospital for about 4 days, and can resume normal activities in a couple of
weeks.
Endometriosis is a condition where the cells that form the lining of the uterus grow into the surrounding areas. Aside from pain, especially during menstruation, during and after intercourse, it can also cause infertility.
About a third of all cases of female infertility are caused by endometriosis where the excess cells occur in the fallopian tubes and block the egg’s passage, or they occur in the ovaries and prevent the release of the egg, or they form in the uterus, ovaries and fallopian tubes and prevent the transfer of the egg to the tube.
Endometriosis is usually treated in one if three ways: watchful waiting, hormone therapy and surgery. Our specialist makes this call depending on your symptoms, age, severity and if fertility is a factor.
What happens during surgery?
The purpose of surgery is to remove as many endometrial implants and cysts as possible, which would relieve pain and improve fertility, and is recommended for women who are still in the child bearing age. It can be done via laparoscopy or laparotomy.
Laparoscopy is the gold standard and preferred method for endometriosis surgery. During the procedure, which is done under general anaesthesia, several tiny incisions are made through which the laparoscope is inserted to give the surgeon a view of your pelvic organs. The specialist then removes the implants and scar tissue using heat. This is a day care procedure, and you do not need to stay in hospital overnight. Recovery usually takes a 1 -2 weeks.
In a Laparotomy, which is only considered in cases of severe endometriosis, the specialist accesses your reproductive organs through a large incision across your abdomen. This is a much more invasive method, and requires that you remain in hospital for several days.
For women who have already had children and have severe endometriosis, there is a third option: hysterectomy to remove the uterus. In most cases the ovaries are not removed, so while your period stops, you will not go into menopause. A Hysterectomy is usually performed through minimally invasive surgery, or in rare cases, open surgery.
Infertility and pelvic pain can sometimes be caused by scar tissue that joins two surfaces that are usually separate, causing the organs it attaches to become twisted or to move from their normal positions. The adhesions may present as thin sheets of tissue or thick fibrous bands. Adhesiolysis is the surgical procedure to remove or divide this tissue and restore normal position and function to the organs involved.
What happens during the procedure?
The procedure is done through laparoscopic methods (with a tiny incision) and takes between 2 – 4 hours depending of the type and extent of the adhesions. It is done under general anaesthesia and you would have to stay overnight at the hospital after the procedure. You can resume normal activities in a week’s time.
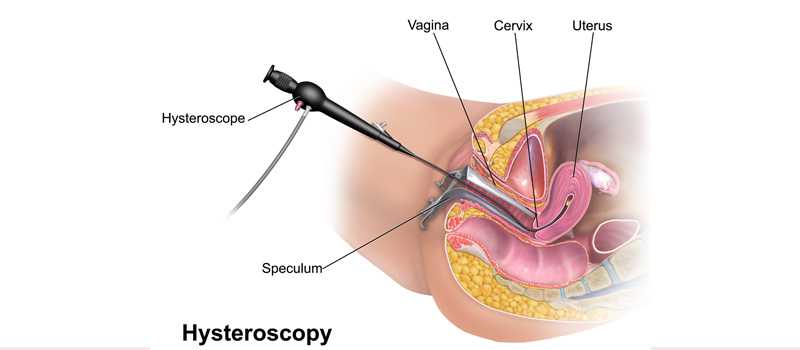
Hysteroscopy is done using a hysteroscope, a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus.
Hysteroscopy can be either diagnostic or operative.
How safe is hysteroscopy?
Hysteroscopy is a relatively safe procedure. However, as with any type of surgery, complications are possible. With hysteroscopy, complications occur in less than 1% of cases and can include:
• Risks associated with anesthesia
• Infection
• Heavy bleeding
• Injury to the cervix, uterus, bowel or bladder
• Intrauterine scarring
• Reaction to the substance used to expand the uterus
What is operative hysteroscopy?
Operative hysteroscopy is used to correct an abnormal condition that has been detected during a diagnostic hysteroscopy. If an abnormal condition was detected during the diagnostic hysteroscopy, an operative hysteroscopy can often be performed at the same time, avoiding the need for a second surgery. During operative hysteroscopy, small instruments used to correct the condition are inserted through the hysteroscope.
When is operative hysteroscopy used?
Surgeon may perform hysteroscopy to correct the following uterine conditions:
• Polyps and fibroids: Hysteroscopy is used to remove these non- cancerous growths found in the uterus.
• Adhesions: Also known as Asherman’s Syndrome, uterine adhesions are bands of scar tissue that can form in the uterus and may lead to changes in menstrual flow as well as infertility. Hysteroscopy can help your doctor locate and remove the adhesions.
• Septums: Hysteroscopy can help determine whether you have a uterine septum, a malformation of the uterus that is present from birth.
• Abnormal bleeding: Hysteroscopy can help identify the cause of heavy or lengthy menstrual flow, as well as bleeding between periods or after menopause. Endometrial ablation is one procedure in which the hysteroscope, along with other instruments, is used to destroy the uterine lining in order to treat some causes of heavy bleeding.
When should the procedure be performed?
We may recommend scheduling the hysteroscopy for the first week after your menstrual period. This timing will provide us with the best view of the inside of your uterus. Hysteroscopy is also performed to determine the cause of unexplained bleeding or spotting in postmenopausal women.
Common procedures performed are:
1- Diagnostic Hysteroscopy
2- Polypectomy
3- Septal resection
4- Tubal cannulation
5- Lysis of adhesions
6- Removal of misplaced IUI